In order to discuss the development of cardiac surgery one should refer to the foundation and evolution of medical and technical ideas, which proved necessary for the cardiac surgeons to practice their profession.
Despite the fact that the fundamental basis of modern science has been attributed to the 17th century in Europe, we should remember that it was the ancient Chinese inventors who far outdistanced Western civilization. As the Europeans, we are deeply convinced that modern science and techniques have their originated mainly in Europe, but there is indisputable evidence that four thousand years BC the Chinese made the discoveries that were then adopted by the European civilization. They manufactured paper, they could use print, powder, wheels, masts, compasses, clocks, ploughshares, wheelbarrows or the decimal system. With regards to the medicine, they were well familiar with blood circulation in the cardio-vascular system and they viewed the heart as the organ responsible for the blood pumping. In China, blood circulation was one of the chief doctrines in medicine and the basis of acupuncture. They distinguished between 28 types of blood pulse, biological rhythms, they were familiar with sex and thyroid hormones and diabetes. They knew visceral and skin reflex and the vaccines against smallpox. An important question arises why did the Chinese, despite their knowledge and experience far more advanced than that of the Europeans, fail to develop their civilization to reach the contemporary European and American standards? Probably, the Chinese did not realize the importance of their discoveries or forgot them because even today it has little knowledge thereof and the West does not feel obliged to discover the whole truth. Perhaps the hierarchical social structure of China at that time impeded the progress, which required personal freedom as well as the freedom of thought and activity. The truth is that no modern cardiac surgery and heart transplantation, space flights or information technology could develop without modern European and, particularly, American science and technology regardless of the knowledge adopted from the Chinese. The issue of the historical interdependence of Western and Eastern cultures should be left to scientists and historians while we should deal with a thorny path between the autopsy of a heart and a precise heart surgery and transplantation performed to preserve human life and health.
Antiquity
From the ancient times, the dream of humanity was to extend the lifespan using all available methods including the treatment of damaged organs. It was believed that the heart was the source of life, soul and thought. In order to kill an enemy, the warriors knew that they should hit him in the very heart. At that time, however, people were unaware of anatomy or physiology of the circulatory system and they were not able to treat diseases and heart injuries. The Chinese emperor, legendary yellow emperor Hwang Ti (2689 – 2599 BC) discovered in his Nei Ching blood and its movement, measured heart rate and, accordingly, defined a prognosis. Based on the observations of nature, course of diseases and religious beliefs, the Egyptians and the Persians practiced the art of medicine and they often recognized disordered functions to the organs. For instance, the Egyptians, who learnt the anatomy during the mummification, believed that the heart had its own life and thoughts and the air flowed through the veins and arteries because they were not able to distinguished between them. In ancient Greece, the development of Hellenic, Aegean and Mycenean culture was linked to the development of philosophy, logic, architecture, body worship and mythology. Apollo was the god of physician and his son, Asklepios, also mastered the art of medicine and he even restored the life back to the dead for which he was killed by Zeus’ lightning. The philosophy combined with the observations of both healthy and sick persons set the beginning of empirical medicine. Asklepios and Hypocrites broke away with the medicine based on religious beliefs and turned to the observation. The growth of knowledge in Egypt, Mesopotamia and India based on the rules of nature, mathematics, physics, astronomy and logic, laid the foundations for the discovery of the surrounding world using empirical methods. Aristotle, a philosopher, taught that the logical thinking should be based on the observation. In Greece, the art of healing was deemed an important branch of philosophy. Thales of Milet maintained that the universe emerged from water and air and he treated people as particles of this universe.
Pitagoras pointed out that the mind resided in the brain. Plato and his pupil Aristotle added to the knowledge of anatomy and, in particular, physiology of heart and circulation but their knowledge was far from complete because they mainly used philosophical approache for their anatomic and diagnostic observations including lung auscultation and percussion. The ancient scientific institute established in Alexandria by Ptolemeus gathered almost entire ancient literature, which unfortunately was set fire by the Arabs in 641 AD. Ptolemeus approved of the autopsy on human remains, which was related to their embalmment. The physicians of the Alexandrian school could measure the pulse but they still adhered to the theory that air flowed through the arteries. They knew the anatomy of the heart, the work of the ventricles and venous valves but they could not understand the blood circulation. They maintained the heart was the breath of blood and that the heart paralysis caused an instant death.
At the beginning, ancient Rome was not god place for the scientists and physicians. It was only in the times of Cicero (I century BC) that the Greek physicians were allowed to employ their medical practices, which at that time laid only in the hands of the Greek. Archigenes of Apamea performed the blood vessel ligation. Claudius Galenus of Pergamum (130-200 AD) was a outstanding physician of his time. He thoroughly described human anatomy and stated that the injured heart was the reason of death. He distinguished between skeletal and cardiac muscles. He carefully described the flow of blood through the heart, the role of valves but he was unable to “close” the circulatory system.
The Middle Ages
The fall of the Roman Empire in 410 AD and the transfer of power to Byzantium resulted in a decline of culture and science in the western part of the empire. Under the Edict of Milan of 313 AD, Christianity was declared the state religion. Churches and monasteries took care of the sick but they were unable treat them. The area of stagnation in science and medicine started in midiaval époque because of the belief that the most important is postmortem spiritual life and earthly life should be the time spent for preparation for heavenly life. Avicenna (980 – 1037 AD) was an excellent Arabic scientist and physician. In 1500 AD in Egypt, diabetes-related polyuria was described on the Ebers papyrus. The medieval Arabic medicine used the ancient and the Byzantium experience in medicine. The medieval physicians discovered the pulmonary blood aeration. Next, the famous universities of Salerno, Paris, Bologne, Montpellier and Padua, where theological studies prevailed, were established.
The Renaissance
The area of dynamic development of natural science began in the Renaissance. The ancient and Arabic medical works were brought back to light and the urge to study and discover started. Gutenberg invented printing. Ambroise Pare’ became known as an excellent surgeon who demonstrated his surgical skills on the battlefield and introduced the vessel ligation. The excellent anatomic works of Leonardo da Vinci and Andreas Vesalius based on the autopsy contributed to William Harvey’s discovery of blood circulation in 1626. Harvey proved that blood circulated from arteries, through arterioles, to veins and Marcell Malpighi observed under a microscope the capillary vessels.
For that moment, a dynamic development of knowledge on circulation physiology and the reasons of diseases started. The progress in clinical medicine got its support in pathological anatomy.
In the 18th century, the surgery and barbery were separated. The academies, colleges and chairs of surgery were established in England, France and Germany. Moreover, the royal surgeon associations were founded including The Company of Surgeons (1745) renamed in 1800 to The Royal College of Surgeons of London, Medical and Surgical College of Berlin and the first surgery clinic established in 1784 in Dresden, Germany. In the Austro-Hungarian Empire, the Joseph Medical and Surgical Academy was established in 1885 in Vienna.
The 19th century saw many prominent scientists whose discoveries gave them a permanent place in the history of medicine, including Jean N. Corvisart, Rene T. H. Laennec, J. Forbes, W. Stokes, T. Hodgkin, A. Fallot, R. Virchow, J. E. Purkinje, L. Galvani, C. Ludwig, C. Bernard, P. Duroziez, M. Raynaud, H. Quincke, A. Fick, Phillip Semmelweis, L. Pasteur, W. C. Roentgen, K. F. Wenckebach, B. Morgagni, W. Hunter, Johann F. A. Esmarch, Jules E. Pean, Emil Teodor Kocher, Jan Mikulicz-Radecki, Ludwik Rydygier, Theodor Ch. Billroth and many others.
After they had acquired knowledge of anatomy, physiology and pathology, the physicians all around the world started to understand the basic reasons of diseases and indicated the ways of treatment. However, it was only the discoveries in basic science including chemistry, mainly organic chemistry, physics with microscopic optics and microbiology that explained the reasons of infectious diseases. Oxygen was discovered (K. W. Scheele 1772), gas exchange in the lungs and the tissues was recognized and biochemistry developed.
The 19th century can be considered as an epoch-making of discoveries. In the case of cardiology and cardiac surgery, the most important discoveries included heart and circulation physiology and the safe reversible cardiac arrest for the time of surgical repair of intracardiac defects. The dreams of outstanding surgeons of that time did not come true given pain, infections, unawareness of the blood groups and blood clotting and the inability to diagnose the patients and precisely locate the pathologic changes that should be removed or repaired. Those who had an enormous contribution in this field include Claude Bernard, W. Eindhoven, Luigi Galvani and Karl Rokitansky. In 1818, James Blundell performed human blood transfusion in a woman who experienced post-partum hemorrhage and in 1828, Johann Diefenbach carried out a successful transfusion of defibrinated blood. Karl Graefe from Warsaw was the first professor of surgery at the university clinic in Berlin. Nikołai J. Pirogov was a field surgeon in the Crimean War and Joseph and John Warren, the brothers, were the first professors of surgery at Massachusetts General Hospital – later the Harvard Medical School the general ether anesthesia was demonstrated at in 1846. Previously, as early as on March 30, 1842, Crawford W. Long, a Georgia surgeon, used ether as an anesthetic. In 1847, Phillip Semmelweis suggested that post-partum fever responsible for 15% deaths in puerperants was caused by infections carried from prosectorium on the hands of obstetricians. The decision to wash hands in calcium chloride solution reduced the rate of complications and proved that Semmelweis was right. After Ludwik Pasteur, the discoverer of wine fermentation bacteria and putrefactive bacteria, Joseph Lister concluded that surgical wounds suppurated due to infections caused by microorganisms and introduced a disinfection with 2-5% carbolic acid solution. He announced his discovery at the Congress of British Surgeons held in 1876 and the new age of surgery, antisepsis and aseptics began. In 1890, Kurt Schimmelbusch equipped the operating rooms with autoclaves and special boxes for the sterilization of surgical materials and instruments. Apart from the hands washed and disinfected with lysol, in 1886 Jan Mikulicz–Radecki introduced to a Cracow clinic cotton gloves, sterile uniforms, caps and face masks. William Steward Halsted, on the other hand, used in 1889 rubber surgical gloves so that his favourite scrub nurse did not suffer due to her hands wounded after lysol disinfection. At the same time, Werner Zoege-Manteuffel in Dorpat (today Tartu) introduced rubber gloves to be used during surgeries.
The 20th century was marked with inventions and discoveries, which were a springboard for dynamic development of cardiology and cardiosurgery, the components of internal medicine and surgery. At that time, the abovementioned specializations were not formally separated and, at the beginning, all physicians were forced to deal with heart and circulation system diseases. E. H. Starling described the rules of cardiac physiology, Werner Forssmann demonstrated cardiac catheterization, Reynaldo dos Santos performed abdominal aortography by dorsal approach, Augustin Castellanos implemented angiocardiography, in 1946, Charles Bailey endeavoured to dilate a stenosed mitral orifice using his finger, in 1948, Russel C. Brock performed pulmonary valvotomy, A. Cournand introduced cardiac hemodynamic measurements, Rene Leriche` performed operations on aorta, F. Mason Sones, Rene G. Favaloro and D. B. Effler performed coronarography, Karl Landsteiner discovered blood groups and Ludwik Hirschfeld participated in the discovery of Rh. Mc Clean’s discovery of heparin in 1915, the discovery of protamine and numerous discoveries in the field of physics, mechanics, electronic and plastics enabled the works on the construction of an extracorporeal circulation machine necessary for the safe reversible cardiac arrest and the supply of oxygen to the important organs of a patient.
Those who provided technical bases for the development of cardiac surgery included Jeger and A. Carrel. The resection of pericardium in constrictive pericarditis performed by E. J. Delorme in 1895 and unsuccessful surgery of mitral stenosis in 1902 can be deemed the beginning of the world cardiac surgery. In 1923, G. Butler cut the stenosed mitral valve but caused the incompetence thereof. In 1925, Sir Henry S. Souttar performed a successful closed mitral commissurotomy (mitral orifice dilation using a finger) and caused only a slight incompetence. In 1929, Werner Forssmann showed the physicians gathered in a lecture room that the right-sided cardiac chamber could be visualized radiographically by the radiopaque urologic catheter inserted via his antecubical vein into the right ventricle. It was the first heart catherization in the world. After this spectacular show, Forssmann applied to Ferdynand Sauerbruch, the most distinguished surgeon of that time, to become his assistant but Sauerbruch refused. Forssman was awarded Nobel Prize and Sauerbruch became infamous for his Nazi sympathies. In 1938, Robert E. Gross ligated patent Botall’s duct and in 1940, Clarence Crafoord performed resection of the coarctation of the aorta.
WWII stopped the development of European cardiac surgery but the field surgeons gained experience related, inter alia, to the removal of bullets and splinters from the heart and the chest. In the field hospitals of Europe and Asia, the greatest material was gathered by the Americans including Dwight E. Harken, Denton Arthur Cooley and Frank Gerbode.
To stimulate the growth of additional collateral circulation in coronary disease, Claude Beck created epicardial and pericardial adhesions using irritating agents such as talc or led the greater omentum to the pericardial sac to “envelop” the heart. Artur Vineberg sunk an isolated vascular bundle with internal thoracic artery in the muscle of the left ventricle to ensure, in the case of myocardial ischemia, the additional blood supply from the systemic circulation. Alfred Blalock (surgeon) and Helena Taussig (pediatrician) made a remarkable contribution to the development of cardiac surgery by diagnosing, determining indications for and performing the operations related to congenital cyanotic heart diseases in small children. These were the palliative operations, which consisted in the combination of the systemic circulation with the pulmonary circulation to improve the oxygenation of blood unable to reach, in sufficient volume, the lungs due to pulmonary artery stenosis in tetralogy of Fallot and in pulmonary hypoplasia or in great vessels transposition. The operation performed for the first time by Blalock and Taussig in 1944 has, in selected cases, been used until today.
For decades more aggressive surgeons performed the first invasive diagnostic procedures including cardiac catheterizations, aortographies, angiocardiographies, transseptal left heart catheterization, cardiac muscle biopsies and artificial pacemaker implantations. At the same time, the surgeons encouraged the internists and pediatricians interested in the diagnostics of circulatory system diseases to undertake such diagnostic activities. After 50 years, the abovementioned activities became a routine and today, in certain cases, the interventional cardiologists can even replace the cardiac surgeons.
In the second half of the 20th century, the world’s leading cardiac surgeons included: Manuel de Jezus Antunes, Michael E. de Bakey, Christiaan Barnard, Sir Brian Barratt – Boyes, Hans G. Borst, Charle DuBost, Viking Olaf Bjórk, H. J. Bretschneider, Alain Carpentier, R. Castaneda, Denton Artur Cooley, D. B. Effler, R. G. Favaloro, E. Fontan, Dwight C. Mc Goon, J. D. Hardy, G. Heberer, Charles Hufnagel, J. W. Kirklin, Walton Lillehei, Domingo Liotta, W. T. Mustard, William I. Norwood, Francis Robicek, Donald Ross, I. H. Rygg, Norman Shumway, Ake Senning, Albert Starr, Juro Wada, Sir Mahgi H. Yacoub and Rudolf Zenker.
POLISH CARDIAC SURGERY origitantes from the general surgery and thoracic surgery which adapted, with a certain delay, also the achievements of the world and European surgery including, in particular, the American, British, German and French surgery.
After the partition of Poland, the development of the Polish surgery was hampered by the foreign administrators. The achievements of the Polish surgeons were neither welcomed nor eagerly published. The international relations were relatively good in the territory occupied by the Austro-Hungarian Empire and the Polish enjoyed greater freedom and were able to participate in the development of the European surgery within the quadrangle of Vienna, Prague, Lvov and Cracow. In the country split among the Prussian, Russian and Austro-Hungarian Empires, the Polish surgery did in fact develop in a foreign state but the scientists and the famous Polish surgeons maintained their national identity and were by no means inferior to their foreign colleagues. They made important discoveries and implementations which were published mostly in a foreign language and, consequently, were not considered as Polish. When they were published in Polish they were not introduced to the world literature. Poland, as a state, did not exist for 123 years and, apparently, “there were no Polish discoveries or achievements in medicine and many other fields.” This fact, which proved sad for the Polish, had an impact on the mentality and decisions of the allied staff and politicians. The Western Europeans’ unawareness of Poland, which disappeared from the map of Europe for 123 years, had a negative impact on defining the borders of the reborn Republic of Poland in 1919. Poland’s struggle to regain independence was manifested in the first congress of the Polish surgeons held on October 16, 1899 in Cracow and organized by most creative Polish surgeon Ludwik Rydygier. 60 surgeons came, almost secretly, from the territories annexed by the three Empires and delivered as many as 40 lectures. So as not to provoke the foreign administrators, the three-day congresses were held each year in Cracow until 1911 but, unfortunately, the name of the Polish Association of Surgeons could not be officially used. The congresses were held, however, under the name: the Association of Polish Surgeons.
A short period of 20 years between the two World Wars saw a dynamic development of surgery. In the II Republic of Poland, the Polish surgeons educated mainly at the universities located in the annexed territories became the heads of hospital departments and university chairs in Cracow, Warsaw, Lvov, Poznań, Gdansk and Vilnius. At the chair of surgery of the John Casimir University in Lvov, Tadeusz Ostrowski and Wiktor Bross performed on September 8, 1935 Poland’s first successful lung lobectomy due to bronchiectasis and, one year later, they removed the lung due to cancer.
THE GREAT WORLD CELEBRATION OF THE 100-TH ANNIVERSARY OF THE ASSOCIATION of POLISH SURGEONS’ held in 1989 in Cracow, in independent Poland, was marked by the absolutely different, elevated atmosphere. The expression of patriotic feelings, historic memory as well as the demonstration of the scientific achievements made by the Polish surgeons over the past 100 years and the significance of the celebration in culture and history was contributed to the Association’s President, Prof. Tadeusz Popiela (Fig. 1). The most impressive fact of this congress was the attendance of more than 500 foreign outstanding surgeons invited as congress guests.
 |
Fig. 1. Prof. Tadeusz Popiela, Rector of Nicolaus Copernicus Medical Academy in Cracow, established in 1979 the Institute of Cardiology with Dept. of Cardiac and Vascular Surgery at the abovementioned Academy. |
After they had controlled pain and surgical infections, the cardiac surgeons faced the necessity of solving the following issues: safe thoracotomy, extracorporeal circulation, reversible cardiac arrest, blood transfusion and blood clotting and the prevention of thromboses and embolisms.
Open chest surgery and endotracheal general anesthesia
In 1905, in Wrocłav Mikulicz – Radecki introduced a low pressure chamber to perform, the first world, surgical procedures inside the chest. It was a complex and extremely difficult method, even for the surgeons. In the same year, a Norwegian physician, in an attempt to rescue his daughter who asphyxiated due to respiratory muscle paralysis in Heine-Medin disease, inserted a rubber tube into her trachea and joined it with a rubber ball which, pressed rhythmically, imitated a natural breath rhythm. Clarence Crafoord developed this method for clinical purposes. The endotracheal intubation has been accepted in the whole world and has successfully been used until today. Meltzer used a tracheostomy tube for artificial respiration. The inhalation anesthetics including nitrous oxide, ether and ethyl chloride evolved to the new, comfortable for both a patient and an anesthesiologist, inhalation, intravenous, conduction, infiltration and epidural anesthesia.
A direct transition from general surgery to cardiac surgery without thoracic surgery proved impossible. It was thoracosurgery that formed a natural bridge between general surgery and chest surgery. It developed dynamically despite of the post-war epidemics of pulmonary tuberculosis, injuries, splinters found in the chest, thoracic empyemas and lung cancer. Previously, the opening of the pleural cavity resulted in death due to pulmonary collapse and suffocation. Gotthard Bulau was the first internist to use in 1875 a closed water-seal drainage for pleural empyema. Consequently, the pressure within the water closed system was balanced and the lung did not collapse. In 1883 in Gdańsk, M. H. Block sewed the wounded hearts of guinea pigs and made an unsuccessful attempt to remove the apexes of both the lungs of his cousin damaged as a result of tuberculosis. In Poland, Franciszek Kijewski pioneered in experimental thoracosurgery. Jan Mikulicz - Radecki of Vienna settled, via Cracow and Konigsberg, in Wrocław where he endeavored, at first with Sauerbruch and then himself, to improve a low pressure chamber for open chest surgeries. After Sauerbruch had left for Berlin, Mikulicz, acting in the territory of Wrocław annexed by the German Empire, emphasized his Polish nationality and joined the world’s leading surgeons recognized as Pole.
Thoracic surgery developed. In 1929, Harold Brunn applied a postoperative drainage of the pleural cavity. In 1932, Churchill made an attempt to ligate the fragments of the pulmonary hilus and in 1933, William F. Reinhoff sewed the main bronchus using single sutures. Rudolf Nissen, Cameron High and Evarts Ambrose Graham performed successful lung resections.
In the 19th century, the human heart was treated as the source soul and as such it was a taboo organ for the surgeons. At the Vienna congress of surgeons held in 1893 Theodor Billroth would say: “A surgeon who dares to operate a human heart cannot expect any respect from his colleagues.” He was very wrong because two years later, on September 9, 1895 at a hospital in Frankfurt am Main, Ludwik Rehn sewed a stab wound of the heart in a 22-year-old man and, consequently, saved his life. Even in Cracow Medical Academy W. Wcislo used to lecture physiology of cardiovascular system warning that surgeon should not touch the heart with knife (“away the knife from the heart”) and “preducted that heart transplantation could never be successful.
Hypothermia
In the 1950s, W. G. Bigelow applied hypothermia. He cooled the body of an operated patient to 28°C to arrest the heart for 5-8 min necessary to close the hole in the atrial septum. Hypothermia protected the tissues against oxygen deficiency during a brief circulatory arrest because the tissue metabolism slows down in lower temperature. At first, in order to perform a surgery using hypothermia and hibernation, a patient was given a relevant anesthetic, covered with ice and bathed in cold water. As the patient’s body temperature reached 28°C, s/he was placed on the operating table. Thomas Lewis, Charles Philamore Bailey, Walton Lillehei and Ernst Derra operated congenital heart diseases using surface hypothermia. In 1958 in Poznań and then in ŁódĽ, Jan Moll (Fig. 2), after his hardly satisfactory experiences related to surface hypothermia, decided to cool the patient’s blood. It was an easier, safer and more efficient method because ventricular fibrillation usually occurred in 28°C. Under extracorporeal circulation, there was no risk of cardiac arrest. Moreover, when compared with the surface cooling, the time necessary to cool the body of a patient to 10°C and warm it with blood was clearly shortened. The abovementioned procedure called for a sufficient heat exchanger, which was constructed by Jan Moll, Franciszek Płużek and Stanisław Szymkowiak at Zakłady Metalurgiczne Hipolita Cegielskiego (Hipolit Cegielski Metallurgical Plant) in Poznań and patented in 1960 under the following name: MPS – 1 (Fig. 3). Jan Moll used deep hypothermia in congenital heart disease repair. After cooling the patient’s body to 10°C, he would completely arrest the circulation for the time necessary to correct a defect, usually for 30 min, and then he would increase the temperature to 37 °C using blood warmed by the heat exchanger.
 |
| Fig. 2. Dr Jan Witold Moll demonstrates the chest x-ray of a child with congenital heart defect. Poznań 1957. |
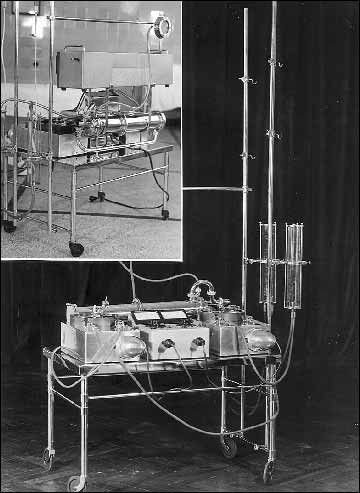 |
Fig. 3. MPS-1 (Moll-Płużek-Szymkowiak) – the first Polish Heart Machine with Heat Exchanger for performing open heart operations under deep hypothermia. |
Extracorporeal circulation, heparin and protamine
The heart-lung machine has been necessary for the safe intracardiac surgery, reversible cardiac arrest, perfusion maintenance and the supply of oxygen to important organs. In 1935, John H. Gibbon began his experimental research on the heart-lung machine. In 1937, he developed the first screen heart-lung machine and was extremely close to applying the device in a person. He said he was prevented by “some madman with a moustache whose mad activities forced him to join the US Army.” He resumed his work after the war and in 1953 made a successful attempt to employ his machine named Total Cardio-Pulmonary By-Pass at the Mayo Clinic. Walton C. Lillehei cooperated with De Wall, Gott and Marco, Earle Kay and Cross and others to improve extremely large and complex machines for extracorporeal circulation. The contemporary membrane oxygenators and machines with always the same Michael de Bakey`s rotating peristaltic pump were separated from the abovementioned machines. It is a replica of a small Juvele rotating pump used during the WWI to perform a field blood transfusion.
The quality and miniaturization of oxygenators and rotating and peristaltic pumps increased hand in hand with the discoveries in organic chemistry – plastics, mechanics and electronics. To be filled, the initial cylinder and cylindrical, plate, helix or screen oxygenators required from five to six liters of blood and were used repeatedly so the cleaning, sterilization and use thereof was complex and time-consuming. Moreover, large volume of blood of the same group but derived from other person used to fill in the machine and the drainage circuit generated, after a few hours of extracorporeal circulation, high hemolysis and significant clotting disorder following from the damage and aggregation of platelets. In 1950, Clark launched the bubble oxygenator. The cylinder bubble oxygenators required defoaming. Otherwise, as a result of the saturation of blood with oxygen, one liter of blood could produce over a dozen of cubic meters of foam. The foam contained in the bubble cylinder was immediately “extinguished” by Dow-Cornig’s Antifoam and the defoamed blood was pumped through the thick filters to the patient’s arteries.
The Polish MPS-1 extracorporeal circulation machine (see Fig. 3) was composed of the heat exchanger and three rotating pumps. It was not provided with the oxygenator – co could be used only in the surgeries in deep hypothermia in the case of which, as the patient’s body temperature decreased and increased, the blood flowed through the patient’s lungs. In 1962, the machine was provided with MPD-3 (Moll-Płużek-Dziatkowiak) cylinder bubble oxygenator with defoamer (Fig. 4) used for a number of years to perform open-heart operations in moderate hypothermia of up to 28°C and normothermia. Rygg-Kyvsgaard oxygenator functioned in a similar manner. Throughout his professional life, Inge Haugdahl Rygg, a Norwegian from Verdal in Northern Norway, worked as a surgeon in Denmark. He never acquired Danish citizenship and, consequently, was not able to become the head of the cardiac surgery department in Copenhagen! As Rygg retired in 1993, his colleagues from Rigshospitalet in Copenhagen wrote “...He never drew any attention to administrative positions...” In 1956, he got in touch with Erik Kyvsgaard, a plastic material specialist and the owner of POLYSTAN, and together they developed a simple, reliable and relatively cheap disposable oxygenator used in the period 1960-1990. Following the modification, the device is still used in the whole world. This single-use device made of plastic and a small metal heat exchanger was easy to use and, what is more important, safe – there was no risk of air microembolisms. Unfortunately, the oxygenator came from the dollar zone and in communist Poland it was subject to rationing.
 |
Fig. 4. MPD-3 (Moll-Płużek-Dziatkowiak) - the first Polish Bubble Oxygenator as a cylinder with defoamer and settling. |
Other extracorporeal circulation machines were developed in Poland including C-TOR 2 artificial heart invented by Zbigniew Lorkiewicz and built at Zakłady Metalurgiczne Hipolita Cegielskiego (Hipolit Cegielski Metallurgical Plant) and the Silesian heart-lung machine designed by Zygmunt Antoszewski. Over a dozen or so years, the machines were used by individual centers in Poland and Mid-Eastern Europe but they were replaced with the new, reliable and safer computerized devices of Stóckert, Kardia, Sarns, Cobe and others. The contemporary computerized extracorporeal circulation machines and small low-prime disposable membrane oxygenators guarantee safety during many-hour cardiac and aorta surgeries though some patients revealed discreet post-operative symptoms of cerebral microembolisms.
The reversible anticoagulation with heparin (McClean, 1915) and restored coagulation with protamine, heparin antagonist, solved the problem of clotting during a few hours of extracorporeal circulation. In the body temperature, the entire heparin is spontaneously inactivated in blood circulation within two or three hours. Due to the use of coumarin derivatives in therapeutic controlled decrease of blood clotting factors, millions of patients with artificial valves facing a risk of thrombotic and embolic complications and the persons exposed to thromboses and embolisms in atrial fibrillation, endocarditis and vessel diseases, especially coronary heart diseases, are able to function.
Cardioplegia
Cardioplegia consists in a sudden and reversible cardiac arrest to enable a precise correction of organic heart disease or a coronary artery bypass graft on a still heart. Many cardioplegic solutions comprising, first of all potassium whose administration in high concentration to the coronary arteries paralyzes the heart’s systolic function, have been developed. In 1957, Donald B. Effler stopped the heart action after he had injected potassium citrate solution to the ascending aorta. In the 1960s, a remarkable contribution in this field was made by H.J. Bretschneider who developed the compositions of optimum cardioplegic solutions. However, it is low temperature which seems to be the most significant factor to stabilize the metabolism in myocytes at the lowest level possible as the enzymatic and metabolic processes within a cell are stopped in the temperature of 4-6°C. When it reaches the temperature of 37 °C, the heart resumes its regular and efficient action. Some centers use the so-called body temperature “warm blood cardioplegia” and some do not use any cardioplegin and perform extremely quick surgical procedures accompanied by the interrupted cross-clamping of ascending aorta for a few minutes.
The artificial heart valves
The artificial heart valves are almost 50 years old. In 1950, Charles Hufnagel was the first surgeon in the world to place an artificial ball valve in the descending aorta of the patient suffering from the incompetence of semilunar aortic valves. In Poland, separated from the West by the Iron Curtain, nobody heard of this event. I learnt of the abovementioned operation at the scientific meeting held in 1958 at the Pathological Anatomy Institute of the Medical Academy of Poznań where I managed the bronchial carcinoma cytodiagnostics laboratory. We were demonstrated the results of autopsy performed on an American of Polish origin who underwent heart surgery in Washington and died of cardiac infarction during his visit to Poland. We were astonished at this ball valve so perfectly sewed and healed to the wall of descending aorta just below the aortic isthmus.
Previously, numerous attempts were made to correct the incompetence of damaged aortic and mitral heart valves but the replacement with an artificial or biological heart valve proved the only efficient method. Dwight Harken implanted an artificial aortic valve in the subcoronary position in seven patients out of whom five patients died. On September 21, 1961, Albert Starr (Fig. 5) performed the world’s first mitral valve replacement using an artificial valve invented by himself and manufactured at the laboratory of M. Lowell Edwards. This cooperation explains the trade name of the valve, namely the Starr-Edwards valve. In the same year, Albert Starr performed a successful artificial aortic valve implantation. His improved ball valves have been used for 40 years. In 1986, I participated in the symposium called The Quarter of Age of Prosthetic Heart Valves in San Diego (Fig. 6) where I saw the museum pieces of more than 500 types and models of prosthetic heart valves. The conclusion reached at that time was unequivocal – there was and there would not be any artificial valve as ideal as a natural valve. No artificial valve could replace a natural valve in a satisfactory manner.
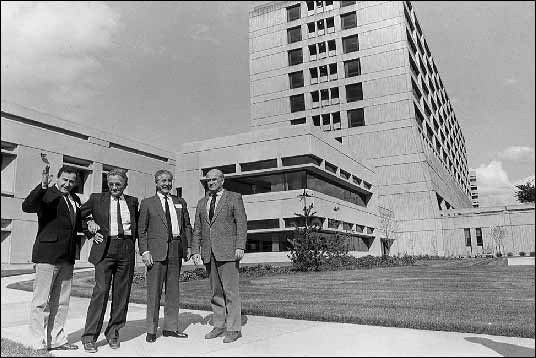 |
| Fig. 5. The representation of the Club of Polish Cardiac Surgeons visits Dr Albert Starr at St. Vincent Hospital and Medical Center in Portland, Oregon, USA. From the left: Dr Janusz Zasłonka – ŁódĽ, Dr Wacław Sitkowski – Warsaw, Dr Antoni J. Dziatkowiak- Cracow and Dr Marian ¦liwiński (President of the Club) – Warsaw. |
 |
| Fig. 6. “A Quarter of Century of Valve Prosthesis” – the meeting in San Diego, 1989. From the left: Victor O. Hall of Oslo, Norway; Juro Wada of Tokyo, Japan; Antoni J. Dziatkowiak of Cracow, Poland and Francis Robicek of Carlotte, N. Carolina, USA. |
In Poland, the first prosthetic mitral valve was implanted by Jan Pruszyński and the aortic valve by Jan Moll in 1964 in ŁódĽ. In this day and age, we implant the artificial heart valves marked by good hemodynamic parameters and failure-free clinical observation for at least ten years.
Moreover, we implant the biological aortic valves, most frequently the homogenous valves, taken from fresh bodies of people who just died, for instance, as a result of traffic accident and were healthy before the accident. Cracow can boast wide experience related to the abovementioned valves. In 1980 at the cardiac surgery department in Cracow, I established the tissue preservation laboratory with deep freezing of up to minus 180°C and the bank of homogenic aortic heart valves. The bank gathered more than 2000 valves out of which I implanted 700 homograft aortic valves in patients suffering mainly from aortic valve incompetence and 80 ascending aortas with valves in patients with the ascending aortic aneurysm. Compared with artificial valves, homogenic valves have many advantages. They are quiet, the patients do not have to take anticoagulants and they are not forced to control blood clotting indixes. However, after 12-15 years, the implanted homografts may be subject to degeneration. In such a case, the incompetence occurs and after 13 year, on average, approx. 6% of patients must undergo reoperation. In 2005 in Cracow, Jerzy Sadowski “inserted” in the aortic root orifice a number of biological heart valves made of equine pericardium, which did not have to be sewed.
Blood and heart surgery without using foreign blood of the donors
The extracorporeal circulation machines are filled with blood of the same group. To be filled, the first heart-lung machines required a few liters of blood. Today, they are filled with blood substitute solutions and diluted blood of patients. Blood management played an important role in the development of cardiac surgery. In 1901, Karl Landsteiner discovered blood groups. Ludwik Hirszfeld and Emil von Dungern established the nomenclature and demonstrated the inheritance of blood groups and in 1940, along with A.S. Wiener, they defined Rh factor. At the early stage of the development of cardiac surgery, up to six liters of blood were used to fill in the heart-lung machine and the entire tubing circuit. The abovementioned blood volume was reduced to zero as a result of the artificial circulation evolution, miniaturization and the launch of the low prime oxygenators and today even the newborn are operated without foreign blood. The extracorporeal circulation machine and the tubes are filled with a blood substitute solution and a surgery is performed using the patient’s own blood diluted to approx. 25% of hematocrit. In fact, a skilled cardiac surgeon should be able to perform a heart surgery without foreign blood. It is possible in approx. 90% of cases but in the case of significant loss of circulating blood volume caused by post-accident hemorrhage, rupture of an aortic aneurysm into the pleural cavity or other reasons, foreign blood transfusion is necessary to save human life. In 1980, Jerzy Sadowski and Zbigniew Samitowski applied the patients’ blood in 60% of open heart operations. The blood taken in two or three portions from a patient scheduled for surgery is stored for him/her at the clinical blood bank.
After heart surgery without any blood has been performed on many patients – the Jehovah’s Witnesses – I am convinced that such procedures are possible and the attempts should be made to carry them out on all patients. At present, it is aimed to eliminate the natural blood transfusion and replace it with blood substitutes. Such a solution is, in every respect, advantageous for the patients because despite a careful examination of blood before and after blood taking, there is a risk of infection with hepatitis C virus (HCV). Moreover, there is a risk of blood clotting disorder and the immunization with transfused blood proteins and the factors which so far have not been discovered.
Coronary surgery
Upon the introduction of coronarography by F.M. Sones in 1962 and a movie demonstration of critical coronary artery stenoses, the surgeons began to perform surgeries directly on the coronary arteries. In 1967, Rene G. Favaloro and Donald B. Effler grafted saphenous vein bypasses from the ascending aorta to the coronary artery beyond the critical stenosis thereof. A borrowed term coronary by-pass entered the Polish medical literature and common speech although its Polish equivalent sounds more elegant: aorto-coronary bridge. In the 1970s, coronarography and coronary surgery represented a real breakthrough in the treatment of coronary disease and cardiac infarction. In 1977, Andreas Gruentzig performed the Percutaneous Transluminal Coronary Angioplasty (PTCA). The procedure consists of non-surgical dilation of the stenosed coronary artery using a balloon tightly attached to the wall at the end of catheter. Under the pressure of a few atmospheres, the balloon “spreads” the hard atheromatous plaques which, in the case of detachment at the site of stenosis, are supported by the stents - the springs saturated with substances used to prevent the coagulation and proliferation of the connective tissue.
In 1957 in Poznań, Jan Moll performed the left heart catheterization. In 1969 in ŁódĽ, Wiktor Iljin performed the first selective coronary angiography. In 1970, Jan Moll performed Poland’s first coronary artery bypasses procedure. As regards the implementation of coronarography, angioplasty and transvascular mitral, aortic and pulmonary valvuloplasty in Poland, a significant contribution was made by Witold Rużyłło of Warsaw and Wiesława Tracz of Cracow.
The term of patency of venous bypasses is shorter than that of arterial bypasses so the surgeons began to use isolated internal thoracic artery whose caliber resembles an average coronary artery diameter. The first procedures of such kind were performed by Ryszard Jaszewski in 1984 in ŁódĽ. Coronary surgeries prevail in the cardiosurgical schedules and represent 70-90% of the operated material. The interventional cardiologists provided with an almost unlimited range of technical equipment dilate the coronary arteries in more than 80% of patients suffering from coronary disease but the post-angioplasty complications and multiple stenoses, especially in the left main trunk and at the arterial branch division, are dealt with by a cardiac surgeon. In the case of coronary surgery, the best solution is to perform an aorto-coronary bypass on a beating heart using the stabilizers to immobilize only the portion of the heart with the anastomosed artery – surgery without extracorporeal circulation, OPCAB.
There has been a revolution in the treatment of coronary disease, especially in acute myocardial ischemia. It was not long ago that a patient with cardiac infarction was laid down in bed and expected to lie still for a number weeks. The period 1998-2000 was marked by a dramatic change in this attitude – the patency of the coronary artery should be restored in the first golden hour so that cardiac infarction does not develop or expand. Another remarkable achievement of the Polish interventional cardiology and cardiac surgery has been the ability to inform and teach the society on how to behave in the case of sudden chest pain, which does not regress following the administration of nitroglycerin: “If you experience the acute retrosternal pain, please do not panic and promptly refer to the hospital able to perform coronarography and restore the patency of the occluding coronary artery.” In Cracow, each taxi driver responds to a person petrified by coronary pain who asks to be quickly driven to hospital in the following manner: “Yes, to John Paul II.” There, at the Cardiology Institute of the Jagiellonian University Collegium Medicum; at the Cardiovascular Disease Department managed by Wiesława Tracz and her apprentices including Piotr Podolec, Tadeusz Przewłocki, Piotr Pieni±żek and Magdalena Kostkiewicz and at the Coronary Disease Department managed by Wiesława Piwowarska and her apprentices including Danuta Mroczek–Czernecka, Jadwiga Nessler, Bohdan Nessler, Grzegorz Gajos and Jerzy Matysek, the patients with acute coronary ischemia are never laid dawn and the staff of the Cardiac and Vascular Disease Interventional Treatment Center and the Institute’s Interventional Cardiology Sub-Division managed by Krzysztof Żmudka accompanied by Artur Kocurek, Wojciech Zajdel and Jarosław Godlewski promptly perform coronarography, locate the coronary artery occlusion and directly restore its patency using stents, if any. The Acute Chest Pain Program I implemented in 1998 in Małopolskie Voivodship is secured by the Cardiovascular Surgery and Transplantology Department managed by Jerzy Sadowski accompanied by Bogusław Kapelan, Piotr Przybyłowski and Paweł Rudziński where the critically ill patients unable to undergo angioplasty and suffering from numerous stenoses of coronary arteries, stenoses of the left coronary artery trunk, cardiac ruptures, ventricular septum perforations and the complications after cardiological interventional procedures performed at the Interventional Center are admitted 24 hours a day. The team of cardio-anesthesiologists managed by Janusz Andres and Rafał Drwiła take care that the patients undergo all invasive surgeries and procedures comfortably and painlessly and quickly restore their health. I and II Cardiology Departments of the Cardiology Institute on Kopernika Street, Cracow, accompanied by the Hemodynamics Laboratory No. 2 execute a similar acute chest pain program managed by Jacek Dubiel and Kalina Kawecka-Jaszcz with Dariusz Dudek.
Heart transplantation
At the end of the 19th and the beginning of the 20th century, many outstanding experimenting surgeons implanted various organs in animals, mainly in dogs, sheeps, pigs and monkeys. In 1905, Charle C. Guthrie and Demichov successfully grafted the head of a dog to the neck of another one. Malicious comments were made by other surgeons who asked why did they fail to sew the third head. In 1902, Alexis Carrel grafted the kidney to the dog’s neck. 1933 saw the transplant of a human kidney. A series of successful kidney grafts as well as the discovery of immunology or rejection and immunosuppression mechanisms laid the foundations for the heart transplantation. Pressed by the cardiologists (“We have been successful with the kidneys; what about the heart?” – they would ask), the cardiac surgeons began an intensive research on the heart transplantation (HTx). In 1960, Richard Lower and Norman Shumway reported a successful orthotopic cardiac transplantation in a dog. In 1966 in Palo Alto, Shumway performed orthotopic cardiac transplantation in a number of calves, which lived for more than six months. His team was prepared to perform the same procedure in people. In the period 1965-1967, Christiaan Barnard, a South African scholar, participated in such experiments carried out in Palo Alto. As he returned to Cape Town he was faced with a following challenge: 54-year-old Louis Washkansky suffering from a serious heart disease and 25-year-old Denise Darvall, who was killed a couple of hours before in a car accident, were taken to Groote Schuur Hospital. On Sunday, on December 3, 1967 at 5:52 AM, the female heart transplanted by Barnard started to beat and the patient woke up. The joy of the patient, his family and the team of surgeons was enormous. It was a miracle of the western civilization.
The whole world learnt of the success and the triumph of humanity over death! The heart could be replaced! However, the joy did not last long. The patient died after 19 days but the beginning was nonetheless marked. Many American and European centers, which had long made relevant preparations, began to transplant the human heart. Several hundred transplantations were performed but the side effects of immunosuppressive therapy resulted in many deaths.
On January 4, 1969 in ŁódĽ, only 13 months after Barnard’s success, Jan Moll (Fig. 7) assisted by Antoni Dziatkowiak (recipient’s table) and Kazimierz Rybiński and Janusz Zasłonka (donor’s table) performed Poland’s first heart transplantation in a 42-year-old male with advanced mitral valve disease and end stage myocardial damage. A young man killed in a traffic accident was the donor. After it had been sewed into the patient’s chest, the heart resumed efficient action but unfortunately, after a few hours, the heart swelled, its action declined and eventually stopped. The joy turned into disaster and the surgeon with his team experienced serious breakdown and many sleepless nights. Years of preparation proved useless. Was it really so? Although we experienced a hate campaign after this unsuccessful transplantation (hundreds of Polish “leading experts” in morality, ethics, civil and penal law, immunology, serology and transplantology began to express their hard opinions), all this criticism contributed to the analysis of formal and legal aspects of the transplantation in Poland. Based on existing legislature, relevant guidelines of domestic specialist supervisory authorities and the regulations of the health resort, which laid the foundations for subsequent transplantations and the adoption of the Polish Act on Harvesting, Storage and Transplantation of Cells, Tissues and Organs in 1997, were gradually implemented. The Polish transplantation act is the most modern act in the world and it provides for an implicit consent of potential donors if the Central Registry does not contain their written objection. In practice, after the Central Objection Registry has been checked, a physician employed by the intensive care department a potential donor died at is not obliged to ask his/her family for approval.
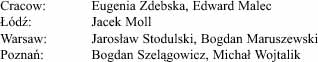
 |
Fig. 7. Prof. Jan W. Moll, Poznań 1964. |
At the same time, in January 1969 in Sapporo, Juro Wada, the most outstanding Japanese cardiac surgeon of that time, performed the heart transplantation and was accused of murder. In Japan, life starts with conception and ends as the heart stops. Wada took the heart from a brain-dead person whose cardiac activity was still maintained.
Moll’s drama produced fruit 16 years later. Over that time, the Polish society and medical circles got accustomed to the transplantation-related issues. Legal and ethical experts wrote many scientific works and made remarkable contribution. Moreover, Cyclosporin A, an excellent immunosuppressive drug invented by accident, was introduced to clinical use in 1980. In 1985, Zbigniew Religa performed another heart transplantation in Zabrze. I was the first person to congratulate him and, given my experience related to the first transplantation in ŁódĽ, I offered my assistance should he become attacked by the “leading experts.” The patient lived seven days but the second stage in the Polish transplantology was marked and subsequent procedures proved successful. In Cracow, it took me a long time to prepare to such a procedure because I still remembered the distress experienced after the transplantation in ŁódĽ. It was only after more than 500 open-heart surgeries had annually been performed by the team that I decided I was ready to face the challenge. On October 21, 1988 in Cracow, I performed, assisted by Jerzy Sadowski and Mirosław Garlicki, the first heart transplantation (Figs. 8 and 9). This success was followed by other successes and the series of 100 successful heart transplantations performed by the team won the scientific reward of the City of Cracow and the Ministry of Health. Now, in 2005, such procedures are the clinical practice and the total number transplantations performed in Cracow stands at 500.
 |
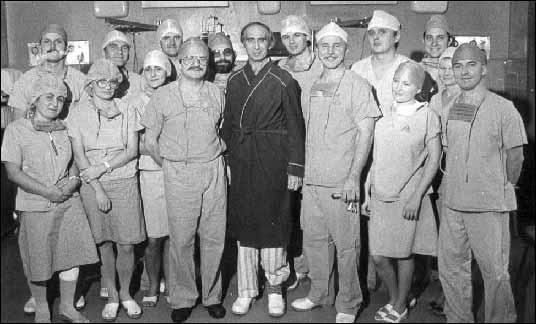
Fig. 8. The first heart transplantation in Cracow performed on October 21, 1988 by Prof. Antoni Dziatkowiak. |
 |
| Fig. 9. The first patient with transplanted heart, Mr Zygmunt Chwirot, 47, of Poznań in 1988. The patient lived for 13 years. |
Heart prosthesis
Within the meaning of a complete replacement of the damaged heart, the artificial heart should be defined as a cardiac prosthesis. The device used to provide a temporary support to a failing heart is composed of the two artificial, left and right, atriums and ventricles, it is electronically synchronized with cardiac activity and it is driven externally. The artificial heart – cardiac prosthesis – is intended for a long-term, total replacement of a damaged heart removed from the chest and it is expected to function “over the patient’s life” Many research centers in the world have developed artificial ventricles to provide a temporary support and permanent prostheses. They function in a similar manner but the artificial heart expected to function “over the patient’s entire life” must meet the following criteria: it must be atraumatic to blood cells, it must not cause hemolysis or thromboses and it must provide for a reliable electronic autoregulation system and power supply system. The artificial ventricles and cardiac prostheses have so far failed to satisfy the researchers and they mainly serve as a bridge until a natural heart is given by a donor.
In the period 1960-1969 at the Baylor University in Houston, Domingo Liotta, an excellent experimental surgical fellow at Michael De Bakey`s service, developed a cardiac prosthesis and recorded good results in calves. At the same university, Denton A. Cooley found himself in a difficult situation. 47-year-old patient, Haskell Karp, was dying due to left heart failure after several cardiac infarctions with a complete atrioventricular block. Cooley asked Liotta to borrow the artificial heart to save the patient’s life and serve as a bridge to transplantation. Without asking De Bakey, the research author, for a consent, Liotta, acting in the best faith, transferred the artificial heart to St. Lucas Hospital operating room and, on April 4, 1969, Cooley performed the world’s first implantation of cardiac prosthesis. At that time, Michael De Bakey attended the congress in Washington. When asked to provide his comment on the event, De Bakey was extremely surprised. The incident sparked off a row. The artificial heart functioned for 64 hours. The patient regained consciousness and he managed to make a will. In June 1969, I attended the I World Heart Transplantation Congress in Montreal and we were positively surprised by a cine-angio film depicting this very patient whose chest contained an artificial beating heart. It was incredible! Later, Cooley implanted a human heart into his body.
The second implantation of cardiac prosthesis was performed in 1982 by J. Coopeland. Afterwards, William De Wries performed a series of successful artificial heart implantations. In 1999, at Texas Heart Institute managed by D. Cooley, I saw and examined two out of thirty five patients with Heart Mate II ventricular assist devices implanted into the abdominal cavity by Branislav Radovancevic. Connected to the heart and aorta, artificial ventricles supported the failing heart for over a year. Encouraged by Michael De Bakey, a NASA engineer developed, following the heart graft, a heart pump using the axial-flow turbine as an example. A similar INCOR device is used in Berlin. Further technical progress is witnessed in this field and more and more advanced heart pumps including JARVIK 2000 and Heart Mate III, which have so far been applied in hundreds of patients, are introduced.
The main problem related to artificial ventricles and cardiac prosthesis includes complex bioelectrical mechanisms in contact with plastics polymers, hemolysis, thrombuses, embolisms, infections and material fatigue. Without going into details concerning the cardiac prosthesis construction, one can say that despite unquestionable achievements, no material absolutely free from the abovementioned defects and complications has so far been developed.
In Poland, Zbigniew Religa has for many years worked on artificial ventricles and cardiac prosthesis and can boast significant achievements in this field. His artificial ventricles are already used at a clinic and successfully function as a bridge to heart transplantation. The electronic control and supply system should be declared as very good.
Plastic materials in cardiac surgery
Carbon derivatives – plastic materials – made an incredible career in every sphere of our life. During WWII, Japan conquered the Asian countries engaged in the production of silk and natural rubber. The Americans were forced to search for hydrophobic material to produce, inter alia, the parachutes and they ordered Dupont and Dow Corning Co. to invent a substitute material. This included Dacron and Teflon, which, in the case of parachutes, proved better than silk, and as a biologically neutral material, proved useful in the production of medical prostheses. The father of American vascular surgery who served during the Corean War (1950–1953) as a consultant of the military health service forbade limb amputation and ordered to apply clamp forceps or ligatures on lacerated peripheral arteries and promptly transfer the wounded to field hospitals where dacron vascular prostheses were successfully used for the first time in the history of field surgery. Dacron, Teflon, Terital, Delrin, Silicon etc. are the synonyms of organic materials, which are still used to manufacture artificial heart valves, vascular prostheses, atraumatic satures and other prostheses applied in surgery, orthopedics and stomatology. Plastic materials conquered the world and made our life easier. However, nobody was able to predict the globe would so hopelessly be littered with those indestructible products of human thought.
Mini-invasive surgeries
Striving for miniaturization and standardization had an impact also on cardiac surgery. Today, the heart surgeries with wide-open chest are being replaced with mini-invasive procedures “through a keyhole” performed with the use of clever endoscopes and surgical tools required for remote surgeries. If it does not increase a risk and the patients so desires, this mini method should used. “Zeus”, “Da Vinci” and other robotic surgical systems make it possible to perform remote cardiosurgical operations using the tools entered through tiny holes to the patient’s chest and controlled by an experienced surgeon. For the time being, such procedures are still at the stage of clinical trials and I do not think they will become a common practice given, for instance, high costs. However, one can expect they will become useful in the areas contaminated by chemical, biological and radioactive agents due to production or transport failures, war or terrorist attack. They will surely prove useful in the space or on a ship floating in the middle of the ocean. Then, a robotic surgical system will perform the surgery controlled by a surgeon sitting at the desk on a distant continent.
Polish thoracic and cardiac surgery after WWII
Before WWII, Poland had 30,000,000 inhabitants and 13,000 physicians. 24,000,000 Polish citizens and 7,000 physicians survived the war. The survivors included a small number of surgeons who engaged in the reconstruction of the country, hospitals and chairs of surgery. During the war, many of them hid in the General Gouvernement and in the woods among the resistance fighters where they helped the sick and the wounded. Jan Moll (who graduated from medicine in 1939) hardly managed to escape the GeStaPo and worked as a young surgeon at the municipal hospital in Radom supervised by Prof. Kazimierz Nowakowski who also hid in that place. After the war, Nowakowski returned to Poznań where he became the head of the Department of Surgery and next of the III Surgery Department located on Szkolna Street 8/12. Jan Moll earned a PhD degree in 1945 and became a senior lecturer at the abovementioned department. During the war, Moll suffered from pulmonary tuberculosis. At that time, tuberculosis was the most serious epidemiological threat in Poland so it did not take long to persuade Jan Moll to establish, at Józef Stru¶ Hospital in Poznań, the Division of Thoracic Surgery to surgically treat active cavernous pulmonary tuberculosis. In 1947, a former Hipolit Cegielski malleable foundry facility located in the garden between Podgórna and Szkolna Streets was adjusted to meet the standards of a chest surgery department and Jan Moll, PhD, became its head. He invited a number of the pre-war physicians and the students of medicine who were enthusiastic about joining this fascinating and adventurous work related to thoracic and cardiac surgery. Those two branches complemented each other and, as the time went by, they did so for the benefit of cardiac surgery.
The students’ scientific association was established at the Division of Thoracic Surgery of Józef Stru¶ Municipal Hospital in Poznań in 1952. I was a member of the abovementioned association. Consequently, in 1952–1956 I was able participate in the Division’s clinical work and assist in chest surgeries. In 1956, I was delegated to complete the specialization in general surgery to the II Division of Surgery of the same hospital located on Podgórna Street managed by Julian Tomaszewski, PhD. I had to complete the first degree specialization in general surgery to start the second degree specialization in thoracic surgery. Moreover, after I had been trained in oncological cytodiagnostics at the Institute of Oncology in Gliwice I established, at the request of Jan Moll and for the purposes of the Division of Thoracic Surgery, the cytodiagnostic laboratory for early detection of pulmonary carcinoma. A high rate of diagnostic compatibility of cytological smear from the bronchial tree with the histopathological results of the lung cancer resection resulted in the establishment, at the request of Janusz Gronowski, another such laboratory at the Pathological Anatomy Institute of the Medical University to provide services to entire Wielkopolskie Voivodship.
I also participated in experimental research on heart-lung machine at the Department of Operative and Experimental Surgery of the Medical University managed by Jan Krotowski and Jan Moll. In 1960, I got a full-time position of an assistant at the Division of Thoracic Surgery and each day I was honored to work supervised by Jan Moll who, as I see it today, developed a liking of me. Consequently, in the second half of the 20th century, I was able to participate in many stages of development of the Polish cardiac surgery, view it with the eyes of a young enthusiast and memorize the most interesting events of the years 1952–2000.
Dzieje kardiologii w Polsce (The History of Polish Cardiology) (PZWL – Medical Publishing, 1994), edited by Jerzy Kuch, contains the chapter written by me and entitled Cardiac Surgery in an Outline. The book sets forth the information on eleven academic cardiosurgical centers active at that time in Poland. I refer the reader to this book and now I will try to recall certain events, comments and observations likely to supplement and revitalize this wonderful history of the Polish cardiac surgery.
In the 1950s, just after WWII, the country was almost totally destroyed. We suffered poverty and Stalinist repressions with all their consequences I am not going to exemplify in this article because the reader will not believe them. Those events were too absurd and often too cruel for the young generation to comprehend. Still, not only were we forced to live in that regime but also we had to take care of our personal and professional development, enter profession, earn a living, acquire additional education, bring up and educate children. Today I view that period of my life as difficult but constructive experience of a young doctor. I was young, bold and, what is most important, I met two wonderful persons, namely my wife Hanna (Fig. 10), maiden name Woch, (today the Jagiellonian University Professor of Pediatrics), a survivor of the Warsaw Uprising, and Jan Moll. As I am writing these words, I would love to pay tribute to these people and thank them for all they did for my personal and professional development and Polish cardiac surgery. I am grateful for the fact that released from the obligation to perform everyday household duties, I was able to devote myself to my passion – cardiac surgery – and undertake undisturbed 27-year-long cooperation with my master, Jan Moll!!!
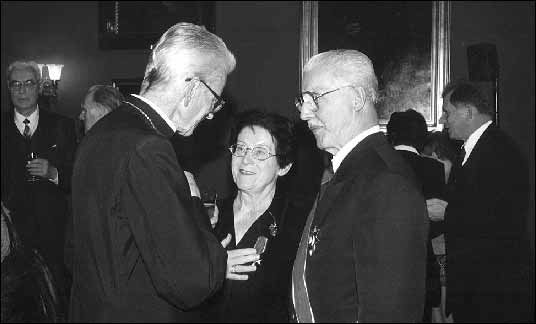 |
| Fig. 10. Cardinal Franciszek Macharski congratulates Prof. Hanna Dziatkowiak on “Commandoria Cross” of the Order of Poland`s Restitution and Prof. Antoni J. Dziatkowiak on his “Grand Cross” of the abovementioned order, 2000. |
In post-war Poland, the pioneering cardiac surgeons included the outstanding general surgeons who fell in love with thoracic surgery and, consequently, “became addicted” to cardiac surgery. These were the enthusiasts of great personality, very brave and ambitious. They had profound knowledge and, as the war survivors, enormous medical and life experience. Among those who made such contribution were Leon Schoege-Manteuffel with his roots in Latvia, Wiktor Bross from Witków near Gniezno in a historical region called Greater Poland, and Jan Witold Moll from Kowalewo near Inowrocław, also in Greater Poland.
Poland’s first cardiosurgical procedures were performed at the Tuberculosis Institute located on Płocka Street 26 in Warsaw by Leon Manteuffel and his team comprising Mieczysław Justyna, Zbigniew Bednarski, Tadeusz Gonta, Tadeusz Koszarawski, Jacek Michałowski, Jan Nowicki, Jan Pruszyński, Wacław Sitkowski, Czesław Turski and Roman Serafin.
Below please find the list of procedures performed for the first time at the abovementioned Tuberculosis Institute:
1948 – Blalock-Taussig shunt and ligation of Botall’s patent arterial duct;
1953 – Mitral commisurotomy;
1957 – Coarctation of the aorta;
1959 – Closure of ASD under extracorporeal circulation;
1960 – Closure of VSD under extracorporeal circulation;
1965 – Implantation of the Starr–Edwards aortic valve prosthesis
1966 – Implantation of the Starr–Edwards mitral valve prosthesis
The heads of the Polish cardiosurgical centers kept in touch with their friends in the West. For instance, Prof. L. Manteuffel would invite to Warsaw Clarence Crafoord with his anesthesiologist, Olle Friedberg, and Ake Senning and Wiking Olaf Bjork, the surgeons from Stockholm. They worked on AGA heart–lung machine with plate or disc oxygenator they brought from Sweden. Their demonstrative operations performed on Płocka Street aroused enormous interest and only the chosen had the honor to observe those innovative heart and aorta surgeries. The Wrocław center, on the other hand, where Wiktor Bross reconstructed after the war (in cooperation with Stefan Koczorowski) and took over in 1946 a former department of Mikulicz–Radecki (Mikulicz–Radecki managed the department in the period 1890-1905 and in 1905, he performed the world’s first open chest surgery (extirpation of mediastinal tumor) using a personally modified Sauerbruch’s low pressure chamber) cooperated with German colleagues, namely Rudolf Zenker of Munich and Ernst Derra of Düsseldorf.
At the Division of Thoracic Surgery of Józef Stru¶ Municipal Hospital in Poznań, Jan Moll performed in 1954 the first mitral commisurotomy and in 1958, he performed spectacular congenital heart disease operations using deep hypothermia of down to10°C. His achievements were not appreciated in Poznań so he left for ŁódĽ. Consequently, Poznań lost its position of a leader in cardiac surgery while ŁódĽ prevailed in this field until late 1980s. In 1959–1979, the II Cardiac Surgery Department of the Medical University of ŁódĽ and, as of 1975, the Cardiac Surgery Department of the Cardiology Institute located on Sterlinga Street 1/3 witnessed a milestone development in Polish cardiac surgery including the improvement of the Polish heart-lung machine, implantation of biological and artificial heart valves, surgical treatment of ascending, descending and abdominal aorta aneurysms, Beck–Moll arterialization of coronary veins, the procedures to provoke the development of collateral circulation in the heart, and coronary artery bypass surgeries.
Moll cooperated with many famous cardiac surgeons, including Karol Siska (Fig. 11) from Bratislava who came to ŁódĽ with his Helix oxygenator on extracorporeal circulation machine.
 |
| Fig. 11. Cardiosurgical Meeting at Smolenice Castle near Bratislava, Slovakia, 1968. From the left: Mrs Izabella Moll (ŁódĽ), Dr Karel Siska (Bratislava), Dr Hanna Dziatkowiak and Dr Antoni J. Dziatkowiak (ŁódĽ). |
In 1959, Jan Moll was awarded a half-year scholarship of the Rockefeller Foundation as a visiting professor. As part of the scholarship, Moll was trained in Minneapolis by Walton Lillehei, in San Francisco by Frank Gerbode and in Houston by Michael DeBakey. I also benefited from the visit to Houston as I was awarded the scholarship at Baylor University College of Medicine where, in the period 1964-1965, I was trained in thoracic and cardiovascular surgery (Figs 12, 13 and 14). It was a break-through event for me and my family. After I had returned from the United States I moved, in 1966, from Poznań to ŁódĽ. In ŁódĽ, we implemented the entire program related to the implantation of prosthetic heart valves, repair of congenital heart disease and aortic aneurysms, operations on thoracic and abdominal aortic aneurysms and all vascular surgeries performed at that time in Houston including, in particular, the surgeries performed directly on the coronary arteries. We managed to convince the leader of the Polish deep hypothermia, Jan Moll, to perform surgeries in normothermia using an oxygenator. Instead of cooling and then re-warming the patient’s body for many hours (it took one day to perform one surgery!) we performed a number of surgeries a day in normothermia and recorded clearly better results.
 |
| Fig. 12. The Doctors’ clinical round at St. Lukes Episcopal Hospital at Texas Medical Center of Baylor University. From the left: Denton Arthur Cooley, PhD, the head of Dept. of Cardio-Thoracic Surgery at Baylor University and his staff: Dr John Allen – a resident, Dr Antoni J. Dziatkowiak - a fellow from Poland; Dr Peter Thiele – a fellow from Germany; Dr Hose Cuadros – a fellow from Peru; Dr Oswaldo Teno Castilho – a fellow from Brasil, 1964. |
 |
| Fig. 13. Forty years after: Dr Antoni J. Dziatkowiak at the same place as in Fig. 7. n 1964, the present (2000) name: Texas Heart Institute in Houston. |
 |
Fig. 14. At Texas Heart Institute - its Director, Dr Denton A. Cooley with visitors Dr Antoni J. Dziatkowiak and Dr Piotr Przybyłowski, 1999. |
The famous people including Walton C. Lillehei (Fig. 15), Frank Gerbode, Rudolf Zenker, Werner Wetzel Klinner, Władimir Iwanowicz Burakovski, W. A. Pokrovski, Donald Ross and Sir Mahdi H. Yacoub visited the Cardiac Surgery Department in ŁódĽ and they performed surgeries, which at that time in Poland were quite innovative.
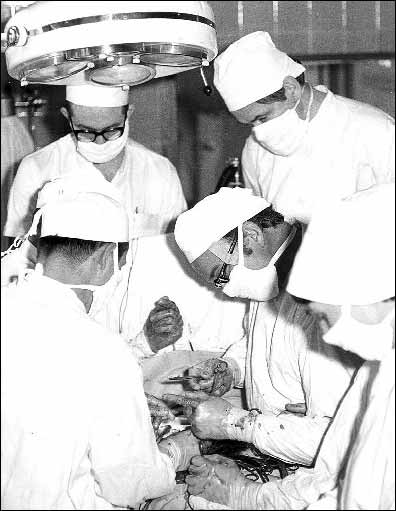 |
Fig. 15. Dr Walton Lillehei of Minneapolis performs an open heart operation in ŁódĽ by invitation of Dr Jan Moll, 1972. Dr Antoni J. Dziatkowiak – as a surgical assistant. |
Years 1960–1990 were marked by a particularly dynamic development of the Polish cardiac surgery. Aware of the fact they fell behind the Western countries, the Polish created new cardiac surgery centers, implemented new surgery methods and increased the number of young and skilled cardiac surgeons. The environment of cardiac surgeons was marked by positive competition – everyone wanted to perform more surgeries, implement modern methods and record better treatment results (Fig. 16). In 1966-1976 in ŁódĽ, more than 500 surgeries under extracorporeal circulation were performed annually. It was also due to competition that an unexpected growth was recorded – from 1800 in 1983 to 30,000 heart surgeries under extracorporeal circulation in 2004.
 |
| Fig. 16. Two friendly competitors in Polish cardiac surgery: Dr Marian ¦liwiński – the Minister of Health and Social Welfare of Poland and Dr Antoni J. Dziatkowiak, at the meeting in ŁódĽ – Nieborów Palace, 1972. |
Below, there is a list of cardiac surgery centers lined up according to the number heart surgeries under extracorporeal circulation performed in 2004. The list takes account only of the centers, which annually perform more than 500 in adults and more than 200 in children surgeries under extracorporeal circulation. The names of the predecessors have also been provided.
The pioneering cardiac surgeons who performed surgeries in adults included: Leon Manteuffel (1904-1973), Jan Moll (1912-1990) and Wiktor Bross (1903-1994).
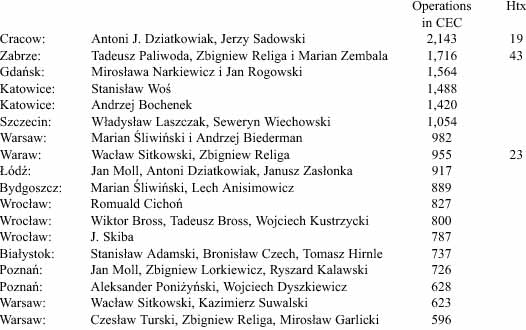
The pioneering pediatric cardiac surgeon was Jan Kossakowski (1900-1979).
Today, we view the years 1960-1990 as the period of the most dynamic quantitative and qualitative development of the Polish cardiac surgery.
As regards the premises, staff and equipment, the conditions resembled those initial ones because the budget did not provide for any funds for improvement and we hardly managed to obtain funds to finance ongoing activities.
I worked with Jan Moll in Poznań since 1952 already as a student of medicine. In 1962, I earned my PhD degree on the basis of my thesis entitled The Research on Metaplasia of the Bronchial Epithelium in Postoperative Material. Janusz Groniowski (Fig. 17), an anatomopathologist, was the thesis promoter and Jan Moll, who performed the lung resection due to the bronchial carcinoma, was the surgical supervisor. Before the operation, I performed the bronchoscopy on the patient and I took cytological smears and sections for histopathological examination. The postoperative morphological analysis of the preparations demonstrated “something” worrying in the mucosal epithelium at the bronchial divisions in the neighborhood of neoplastic change. I managed to prove that the mucosal epithelium converted, as a result of metaplasia, from the multilayered cylindrical to stratified squamous epithelium. Later, my discovery was deemed the introduction to the development of squamous cell carcinoma. In 1966, I accepted the offer of employment at the Medical University of ŁódĽ where I earned my associate professor degree on the basis of my thesis entitled The Experimental and Clinical Research on Heterogenic Aortic Heart Valves. The experience gathered as I participated in numerous cardiac and vascular operations at Texas Medical Center in Houston (30 surgeries a day!) supervised by Michael De Bakey (Fig. 18) and Denton Cooley and clinical implementation of the American novelties in ŁódĽ enriched my knowledge and personality and shaped previously taken ideas. I managed to incorporate most of the abovementioned ideas in Cracow I moved to in 1979 after 27 years of wonderful professional experience with Jan Moll (Fig. 19). In the mean time I and my wife Hanna, we visited Holly Father in Vatican (Fig. 20).
 |
Fig. 17. Dr Antoni J. Dziatkowiak with his PhD thesis promotor, Prof. Janusz Groniowski. Poznań 1962. |
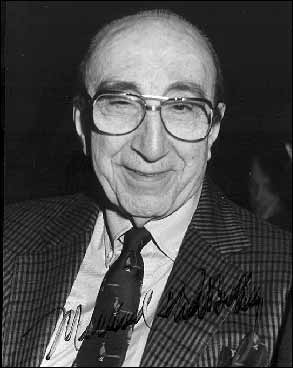 |
Fig. 18. Dr Michael DeBakey “The Texas Inventor and Cardiosurgical Tornado.” |
 |
| Fig. 19. At “the divorce party” on May 31, 1979 in ŁódĽ. After 26 years of splendid cooperation, Dr Antoni J. Dziatkowiak leaves his teacher and master - Prof. Jan W. Moll, for Cracow. |
 |
| Fig. 20. Doctors Antoni and Hanna Dziatkowiak at the private audience by His Holiness John Paul II at Vatican 1980. |
Development of cardiac surgery in the royal capital city of Cracow
The beginnings of cardiac surgery in Cracow date back to 1938 when Jan Glatzel (1888-1954) performed a resection of the heart sac in constrictive pericarditis. At the II Chair of Surgery, Kornel Michejda (1887-1960) and Jan Oszacki (1915-1982) demonstrated interest in heart surgery since 1964. Leon Tochowicz invited Wacław Sitkowski who, in the period 1964-1974, commuted from Warsaw to Cracow to “red surgery” located on Kopernika Street where, assisted by Jerzy Lewandowski, he performed surgeries on patients with selected acquired heart diseases diagnosed and prepared for surgery by Leon Tochowicz, Władysław Król, Tadeusz Horzela and Jerzy Tabeau. These were the surgeries without hypothermia and extracorporeal circulation; i.e. the surgeries on a beating heart. In 1970, the Cardiac Surgery Division was established at the II Chair of Surgery, which has never acquired the status of a separate unit. In 1952, at the III Chair of Surgery at Gabryel Narutowicz Hospital, Michał Juszczyński performed Poland’s first mitral commisurotomy managed by Jerzy Jasieński. At the same time, Cracow witnessed a dynamic development of children’s cardiac surgery managed by Jan Grochowski accompanied by Wacław Sitkowski and Irena Smólska from Warsaw, Eugenia Zdebska, William Imon Norwood, Marek Wites, Janusz Skalski and Edward Malec.
The internists and cardiologists of Cracow, both at academic and municipal health care centers, dynamically developed the heart disease diagnostics and urgently needed a cardiac surgeon to perform surgeries on many patients prepared to undergo surgeries in Cracow. Various options concerning staff and location were considered.
In Cracow, the development of first thoracic surgery and then cardiac surgery department was witnessed at Dr Anka (Helena Wolf) Cracow Specialist Hospital and, as of 1990, John Paul II Cracow Specialist Hospital whose Division of Thoracic Surgery proved necessary to perform surgeries on patients selected from 400 patients treated due to tuberculosis and pulmonary carcinoma at five phthisiological and pulmonological divisions of this Hospital. The history of the abovementioned Hospital located in Pr±dnik District of Cracow dates back to the 13th century and is related to Sławków hospital established in 1298 by Jan Muskat, the bishop. In Biały Pr±dnik District of Cracow, the construction of Miejskie Zakłady Sanitarne (Municipal Medicosanitary Facilities) started in 1913 and was completed in 1917. The abovementioned Facilities comprised a disinfection plant, an isolation ward, a sanatorium for the patients suffering from tuberculosis and a sanatorium for the patients suffering from scarlet fever, which, after certain arrangements, comprised the thoracic and cardiac surgery divisions. Józef Gasiński (1903-1989) became the first head of the Division of Thoracic Surgery and held this position in the period 1947–1950. Next, Władysław Laszczak (1907-1992) served as the head of the Division of Thoracic Surgery in the period 1952-1960. In 1960, Stefan B±k (1917-1981) became the head of the Division of Thoracic Surgery but held this position only for one year. After Władysław Laszczak had been dismissed (he became the head of the newly established Thoracic Surgery Department of the Medical University of Szczecin), Zbigniew Drzewski, an experienced thoracic surgeon from the sanatorium in Bystra ¦l±ska, won the competition for the position of the head of the Division of Thoracic Surgery at Dr Anka Hospital but the post was nonetheless taken by Michał Juszczyński. On the basis of the abovementioned Division of Thoracic Surgery, Juszczyński created the Center of Thoracic and Cardiac Surgery where he performed, under the patronage of Jan Moll and assisted by Antoni Dziatkowiak who commuted from ŁódĽ to Cracow, over a dozen of heart surgeries under extracorporeal circulation.
On June 2, 1979, invited by Tadeusz Popiela, the Medical University Rector, the apprentice of Jan Moll, Antoni Dziatkowiak accompanied by the team comprising Wiesława Tracz, a cardiologist, Barbara Koziorowska and Roman Wirpszo, the anesthesiologists, Jerzy Sadowski, a surgeon and Wanda Jarosik, maiden name Dziatkowiak (Fig. 21), a perfusionist (extracorporeal circulation) who received modern education supervised by Homan van der Heide in Groningen (1976-77) and Jan Nauta in Rotterdam (1978– 79), the Netherlands, came from ŁódĽ to Cracow.
 |
| Fig. 21. Dr Wanda Jarosik, maiden name Dziatkowiak, „running” the heart-lung machine for open heart operations at the Dept. of Cardiac and Vascular Surgery of the Institute of Cardiology, Jagiellonian University Collegium Medicum, 1980. |
In 1979, the Cardiology Institute comprising ten departments and divisions was established at the Medical University of Cracow. Antoni Dziatkowiak became the director of the Cardiology Institute and the head of the Cardiovascular Surgery Department. Michał Juszczyński became a deputy clinical head of the institute and the head of the Thoracic Surgery Department newly established at the Institute. He was also appointed the assistant professor at the Medical University. The Institute has its two Cardiology Departments located on Kopernika Street. The other units together with the Cardiac Surgery Department operate at Dr Anka Hospital. The open-heart surgeries in patients previously qualified for surgeries at the Cardiac Surgery Outpatient Clinic in ŁódĽ were immediately applied. In October and November 1979, 20 open-heart surgeries were performed and no complications were recorded. In the subsequent years, the number of open-heart surgeries performed in a year increased and hit 1000 but the quality of premises and equipment did not meet the requirements of modern cardiac surgery. This fact was confirmed by Tadeusz Popiela, the Medical University Rector, and the city authorities. Thus, I suggested the construction of the new house for cardiac surgery department at Dr Anka Hospital. The project failed due to martial law, which was a waste of time also in the case of improvement of treatment conditions. It should be reminded that the facility the cardiac surgery was located at in 1979 was erected in 1917 as the facility for children suffering from scarlet fever. During and after WWI, this disease raged not only in Cracow. The facility was furnished with 100 beds, two bathrooms with two lavatories and one operating room, which could serve rather as a wound dressing room. My efforts to include the construction of the new department in the state investment program were rejected with elegant words and letters, which pleased many of my “friends.”
This Cracow event resembled that experienced in 1882-1887 by Jan Mikulicz – Radecki who became the Jagiellonian University professor of surgery but the conditions he was forced to operate in were, given the standard expected at that time, extremely poor. It was manifested in the inaugural lecture delivered by Mikulicz who hoped “the government would promptly commence the approved construction of the department able to meet contemporary standards” but he realized that “in any case they would be forced to spend several years surrounded by the old walls.” The efforts to erect a new department drove his activities in Cracow and they contributed to both his success and failure. March 1883 saw the establishment of a special committee comprising a number of the medical faculty members. The task of the committee was to negotiate with the Vienna ministry about the provision of funds necessary to finance the construction of the department. However, the committee’s efforts took too much time and were inefficient. Mikulicz gave up the chair in Cracow and accepted the chair of surgery in Konigsberg in 1887. In 1893, he left Konigsberg for Wrocław. After one hundred years, the history, which in that case involved the cardiac surgery department, repeated itself in an almost identical manner. Everyone wanted, everyone offered their earnest help, the committees adopted resolutions, I received beautiful letters of support and was offered assistance but under the surface I could sense the inability. One hundred years later, in 1983, the delegation of the Medical University Rector and the President of the City of ŁódĽ came to Cracow to enforce the agreement concluded with the authorities of the city of Cracow in 1979. Under the agreement, the academic and administrative authorities of ŁódĽ gave their contingent consent for my temporary transfer to Cracow until the post of the head of the ŁódĽ Cardiac Surgery Department was made vacant by Jan Moll. Moll retired in 1983. I decided to accept the offer and return to ŁódĽ. It is worth mentioning that at that time, the specialists who earned their assistant professor degrees comprised the staff and state authorities were in a position to decide about the “suggested” distribution of managerial positions. From that moment, my Cracow experience began to differ from that of Mikulicz. The authorities of Cracow undertook decisive activities to keep me. The heads of Health and Social Care Division of the Municipal Office of Cracow, Zdzisław Wójcik, PhD, and Mieczysław Wilczyński, MA, were ordered to include the project entitled The Expansion and Upgrading of the Cardiac Surgery Department at Dr Anka Hospital in the investment scheme. Previously, in 1982, the senate of the Medical University resolved to include the construction of the cardiac surgery department in the scheme concerning the newly designed Medical University clinical hospital in Prokocim District of Cracow, which, after 25 years, is still in statu nascendi. I can suppose the efficient execution of the investment concerning the establishment of the new house for cardiac surgery department in Cracow was owed to three broadminded people, namely Tadeusz Popiela, the Medical University Rector, Apolinary Kozub, the Chairman of the National Council of the City of Cracow and Tadeusz Salwa, the Mayor of the City of Cracow.
The establishment of the new house for cardiac surgery department in Cracow was my dream based on my observations of the most modern cardiac surgery centers in the world including Texas Medical Center, UCLA Medical School, Stanford Medical Center, Rochester Medical Center, Hannover Medizinische Hochschule, Deutsche Herz Zentrum in Munich and Berlin, Monaco Heart Institute and Genolier Heart Center. The technical and economic assumptions and technical design were quickly prepared in stages and, owing to the efforts of Bogumił Korombel, MA, the head of the Cracow Expansion Board, the design was approved at the road session of the Committee for the Evaluation of the Ministry of Health Investment Projects during one afternoon in Cracow. The construction started in December 1988. The eight-meter deep excavations were made, pad foundations were cast over the area of 30x80m and the frogs began to croak. In the first quarter of 1989, the construction stopped due to the budgetary collapse of the State experienced during the Velvet Revolution. In this dramatic situation, Antoni Dziatkowiak and his patient after the implantation of an artificial aortic valve, Karol Paluch, MA, decided to establish COR AEGRUM Foundation for the Development of Cardiac Surgery. The idea originated in 1989 in the head of the abovementioned man after cardiac surgery who, as any other patient, was forced to join the line to a corridor bathroom at 4:00 AM.
The foundation was established on April 23, 1990 in the Metropolitan Curia and 19 founders signed the notarial deed. His Eminence Cardinal Franciszek Macharski agreed to become the honorary chairman of the Foundation’s Council. Antoni Dziatkowiak bacame the chairman of the Foundation’s Council and Karol Paluch, MA, was appointed the Executive Board President. It was difficult to register the Foundation because the old authorities suspected it of revolutionary activities and the new authorities – of the resistance against communism. As usual, it was the grateful patients who offered their help – the Court in Warsaw Praga District finally registered the Foundation and ordered to open a bank account at BPH. At the very start, Janusz Quandt, the president of the abovementioned bank, transferred the amount of PLN 2bn to the Foundation’s bank account. We were extremely inspired by his decision and during one year we managed to gather from our wonderful donors the funds sufficient to resume the works, reach the seventh floor within two years and deliver the facility of 60,000 cubic meters in a rough, closed condition. We were all astonished at this success.
It could seem there were no reasons to get so excited. One could say it was just an ordinary construction like any other and the physicians should not get so enthusiastic about it. But, for a number of reasons, it has been an extraordinary construction (Fig. 22). First, it was the idea of the two disobedient enthusiasts who refused to give up and started to execute the project contrary to any logic. At that time it was difficult to believe in a successful execution of the abovementioned project. In 1990, at the beginning of the system transformation and dismantling of the bonds of cooperation, many advanced constructions of the Polish hospitals, including the hospital in Podgórze District of Cracow, were stopped. Second, the donors from Cracow (Fig. 23), entire Poland and foreign countries believed us and due to their generosity, the facility rose from the foundations by the deadline. Third, there was a number of wonderful, accidental coincidences in favor of the project. St. Sister Faustyna (Kowalska) beatified on April 18, 1993 and canonized on 30 April, 2000 by John Paul II, was treated at Dr Anka Hospital in 1936-1937 and 1938. In 1990, the Holy Father agreed to take patronage of the hospital and gave his consent for the hospital to assume his name. In 1993, the Medical University returned to its previous proper place at the Jagiellonian University as Collegium Medicum. The appeals, petitions, requests and responses produced fruit and the good results of thousands of cardiac surgeries created a favorable atmosphere around cardiac surgery in Cracow, which was another factor in favor of the construction.
 |
| Fig. 22. The new house of Dept. of Cardiac and Vascular Surgery under construction in 1993.On the left: The old pavilion and the cars do not exist any more in 2006. |
 |
| Fig. 23. The Donators watch their names carved in the marble wall at the main “Papas Hall” of the new house of Dept. of Cardiac Surgery; they offered their financial and any other support for the project concerning the establishment of the new house. |
The first heart transplantation was performed in 1988 in Cracow and the next series of 100 successful heart transplantations won the scientific reward of the City of Cracow (Fig. 24) and the Ministry of Health. In 1992, Kazimierz Barczyk, PhD, an MP in the Sejm the Republic of Poland, submitted an interpellation to the Speaker and, consequently, further construction of the cardiac surgery department was included in the central investments financed from the state budget. On March 22, 1995 in the Metropolitan Curia, 21 governors and 12 Church hierarchs accompanied by the representatives of the Central Planning Office, the Ministry of Finance (Fig. 25) and the Sejm Sub-Committee for the Control and Assessment of Central Investments took part in the meeting convened by His Eminence Cardinal Franciszek Macharski and Antoni Dziatkowiak. The aim of the meeting was to discuss the share of voivodships in the cost related to the construction completion, the furnishing of the new cardiac surgery department and the acquisition of funds necessary to finance the project. The patients from the country underwent surgeries at the department in Cracow and the cost was incurred exclusively by the Governor of Małopolskie Voivodship. In June 1995, the state budget amount allocated to the construction doubled. It should be stressed that regardless of the organization and investment activities related to the department’s construction, the department’s staff performed everyday exhaustive cardiac surgery activities in the old facility and managed to each year increase the number of cardiac surgeries, maintain the position of the country’s leader, both in terms of quality and quantity and annually perform over 500 cardiac surgeries more than other centers. Many foreign medical and administrative delegations came to the cardiac surgery department in Cracow and were astonished at the ability to perform 1500 surgeries a year in such difficult conditions. The situation gave rise to a ranking and, consequently, in 1987 Cracow obtained two x-ray angioscopes to perform coronarography. As a result, the physicians were able to quickly diagnose and perform surgeries on the patients facing a risk of myocardial infarction. The number of coronary surgeries clearly increased. Maria Hoffman (Fig. 26), the head of the National Institute of Cardiology and the state’s specialist in cardiology at that time, made an enormous contribution to the development of the Polish cardiology and cardiac surgery. She managed to encourage the cardiac surgeons, especially the cardiac surgeons from Warsaw and Cracow, to engage in friendly competition (see Fig. 16), which resulted in the great increase in the quality and quantity of cardiac surgeries. She treated cardiology and cardiac surgery as two equal specializations, which complement one another, and, pursuant to their achievements and the department’s abilities, she equipped them with highly specialized equipment and wearing parts.
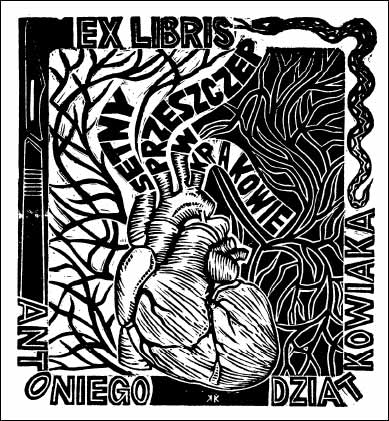 |
Fig. 24. “EX LIBRIS” of Antoni Dziatkowiak’s 100 successful heart transplantations in Cracow (drawing by Krzysztof Kmieć). |
 |
| Fig. 25. Business meeting to discuss the necessity of financing the investment related to the New House of Cardiac Surgery in Cracow from the state budget, 1995: Ms Halina Wasilewska-Trenkner, Vice-Minister of Finance of Poland, Prof. Antoni J. Dziatkowiak, Director of Dept. of Cardiac and Vascular Surgery in Cracow, His Eminence Cardinal Franciszek Macharski, Metropolitan of Cracow and Karol Paluch, MA, the President of COR AEGRUM Foundation for Development of Cardiac Surgery. |
 |
| Fig. 26. Prof. Maria Hoffman receives the diploma and statuette of COR AERGRUM in recognition of her outstanding and deserved contribution to the development of Polish cardiology and cardiac surgery, 1997. |
Despite obstacles, the construction of the new house for cardiac surgery department, already at John Paul II Hospital, progressed. If we consider the reality and project feasibility at that time, an important and positive role was played by His Eminence Cardinal Franciszek Macharski. During the conversation held in 1990, His Eminence recalled the Prince and Bishop Committee established in 1917 by Prince Archbishop Stefan Adam Sapieha to gather funds and erect in Bystre the sanatorium for children suffering from osteoarticular tuberculosis. This beautiful facility has served the sick children until this day. “Why don’t we apply this example in Cracow?” – the Cardinal would ask. Offered a moral support by its honorary chairman, COR AEGRUM Foundation for the Development of Cardiac Surgery managed to complete the abovementioned task.
In 1995, I learnt about the 8th Eucharistic Congress to be held in two years in Wrocław. According to their tradition, such congresses are summarized and each time closed by the popes. The idea originated in my head to invite John Paul II and ask him to consecrate the newly established department. The idea was unusual but feasible given the favorable events including the beatification and prepared canonization of Sister Faustyna Kowalska, a former patient of John Paul II Hospital, and the awareness of the fact that the Pope might take a chance to visit his beloved Cracow and bless the sick at the hospital bearing his name. Thus, in 1995, I went to the Metropolitan of Wrocław, His Eminence Cardinal Henryk Gulbinowicz, and submitted our request to the host of the congress. At first, the Cardinal got angry and deemed the idea mad because the Pope would arrive only for a few hours to participate in the congress closure and return to Vatican promptly after. It was a difficult though charming conversation over his delicious liqueur but I returned to Cracow without any decision. However, the conversation proved extremely fruitful. Via the Metropolitan Curia of Cracow, the hospital sent the invitation to the Holy Father accompanied by the request to consecrate the new cardiac surgery department and visit the patients at John Paul II Hospital. Owing to the support of His Eminence Cardinal Franciszek Macharski, the invitation was accepted and entered into the schedule of the Holy Father’s pilgrimage to Poland in 1997 contained in the White Book. At that moment, the miracle happened!!! Poland had never witnessed the completion of the department’s construction, the reconstruction of the hospital’s entire, obsolete infrastructure dating back to the times of His Majesty Franz Joseph and the hospital’s embellishment performed in such an efficient manner. As a result of the Pope’s visit scheduled for June 1997, the construction and completion works were completed at least two years earlier. The visits paid by Vatican’s and Poland’s secret service forced us to completely replace the equipment and improve the hospital’s facilities. Mainly for the safety reasons, the abovementioned activities had to be completed before the Pope’s arrival. The hospital benefited from the Pope’s visit almost in the same manner a city benefits from the organization of the Olympic Games.
The engagement of the hospital’s entire staff and the working teams of the cardiac surgery department, from the ward maids, nurses, MAs to assistant professors and professors, was impressive. After the construction had been completed, they cleaned the rooms, halls and corridors until they shone. The Holy Father was to be welcomed in the main hall of the new cardiac surgery department covered with beautiful cream-colored marble.
On June 9, 1997, the house and everything was perfectly prepared (Fig. 27). The secret service checked everything and everyone. As I was waiting for the Pope, I entertained the VIPs in my office. In the meantime, I practiced my welcome speech. Suddenly, just a dozen of minutes before the papamobile’s arrival at the hospital, I was told there was neither noaspergillum nor holy water in the hall! A table, noaspergillum and a utensil with the holy water were immediately brought from the Sister Faustyna Chapel.
 |
| Fig. 27. The new house of the Dept. of Cardiac and Vascular Surgery and Transplantology ready to admit patients in 1997. On the left: The old pavilion renovated in 1999 for Heart and Lung Transplantation. |
Before the Pope’s arrival (Figs 28 and 29), I watched the videos depicting welcome speeches delivered during his previous pilgrimages to the world. I noticed that quite frequently, the Holy Father, pensive and supported by his hand, did not listen to the greetings. I decided that in order to attract at least some attention of His Holiness I would maintain close eye contact. It was easy to achieve given a small size of the greeting hall. The group of VIPs who greeted the Holy Father included, inter alia, old friends of Karol Wojtyła. I was honored to introduce them to the Holy Father by their first and last names (Figs 30-32). They bowed and the Pope responded in a similar manner. The Pope listened attentively to a further part of my speech and, after a ceremonial prayer, he consecrated the department and uttered the following words: “May it serve!” (Fig. 33). He blessed the patients after cardiac surgeries, including the patients after heart implantation. Among the patients, there was Ms Urszula holding two-year-old Damian (Figs 34 and 35) whom she delivered three years after the heart transplantation and Priest Marks. As he heard the last name, the Pope asked: “Perhaps Charles?” In the hospital’s courtyard, the Holy Father delivered a boosting speech to the patients and the health service representatives who came from the entire country.
 |
| Fig. 28. June 9, 1997. The guests waiting for the arrival of John Paul II. From the left: Priest Prof. Józef Tischner, Profs Hanna and Antoni Dziatkowiak, Rector of Collegium Medicum, Prof. Stanisław Konturek, Rector of the Jagiellonian University, Prof. Aleksander Koj, Melania Jakimowicz, PhD and ProRector of the Jagiellonian University, Prof. Stanisław Hodorowicz. |
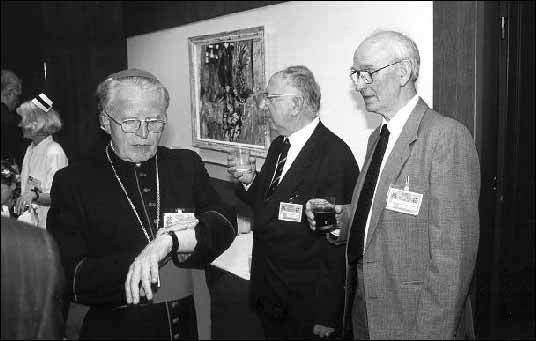 |
| Fig. 29. Fig. 29. The three former patients of the Dept. of Cardiovascular Surgery awaiting for the Pope’s arrival: The Archbishop of Częstochowa, Stanisław Nowak, Marek Skwarnicki, a writer and Karol Paluch, the President of COR EAGRUM Foundation. |
 |
Fig. 30. Prof. Antoni J. Dziatkowiak welcomes His Holiness John Paul II in the main hall of the new Dept of Cardiac Surgery on June 9, 1997. |
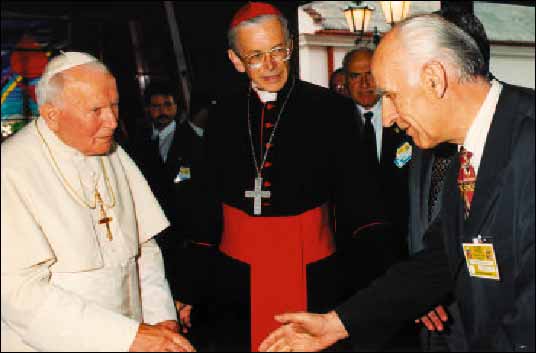 |
| Fig. 31. The Rector of Jagiellonian University Collegium Medicum, Prof. Stanisław Konturek, welcomes the Pope accompanied by Cardinal Franciszek Macharski. |
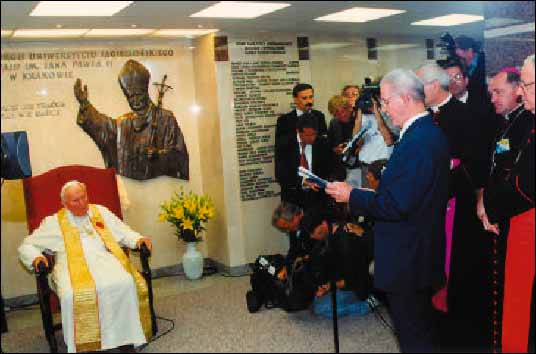 |
| Fig. 32. Prof. Antoni J. Dziatkowiak delivers a welcome speech to Holly Father John Paul II in the main hall of the New Dept. Behind: Archbishop Kazimierz Nycz (Cracow) and Cardinal Angelo Sodano (Vatican). |
 |
| Fig. 33. Holly Father John Paul II assisted by S.E. Mons. Piero Marini consecrates the New Dept. of Cardiac Surgery and blesses the patients in the main hall. |
 |
Fig. 34. John Paul II blesses Ms Urszula and her one year old son Damian whom she delivered three years after the heart transplantation. |
 |
Fig. 35. In 2005, nine-year-old Damian accompanied by his mother Urszula and his father, took his First Holy Communion. He is the only boy in the world born of a woman with new heart who has been blessed by the Pope. |
The anniversary of this day is joyfully celebrated at our hospital. For me, that day was the unforgettable wonderful experience kindly given by the history. I was satisfied to decide that on that day, I, the entire team of cardiac surgeons (Fig. 36) and my family had their five minutes in history (Figs 37-39).
 |
| Fig. 36. The Department’s cardiosurgical and transplantation staff in 1997. The first row from the left: Grzegorz Marek, PhD, Maria Bożek, MA, Grażyna Sokół, PhD, Prof. Jerzy S. Sadowski, Prof. Antoni J. Dziatkowiak (Head of Dept.), Roman Pfitzner, PhD, Marta Biernat, PhD, Melania Jakimowicz, PhD, Roman Tlałka, Dr of Eng. |
 |
Fig. 37. “EX LIBRIS” of John Paul II, the Polish Pope. |
 |
Fig. 38. “EX LIBRIS” of the Dept. of Cardiac and Vascular Surgery of Jagiellonian University made to commemorate the visit of John Paul II to Cracow on June 9, 1997. |
 |
Fig. 39. 1997. Christmas Greetings sent from Vatican by Cardinal Stanisław Dziwisz with greetings from John Paul II to COR AEGRUM Foundation. |
At the new cardiac surgery department in Cracow, thousands of patients undergoing surgeries due to cardiovascular system diseases enjoy comfortable conditions. Moreover, the new ability to quickly diagnose the patients, prepare them for procedures, perform surgeries in a safe manner and apply the postoperative treatment has been provided. It is also the medical staff who enjoy comfortable working conditions. In Cracow, Małopolskie Voivodship and the entire country, the department is recognized as the world center of modern medicine.
The department occupies the area of 60,000 cubic meters and is five times bigger than the old facility. The admission and resuscitation rooms, the department’s administration, the executive board of COR AEGRUM Foundation for the Development of Cardiac Surgery, the Cardiac and Vascular Disease Interventional Treatment Center and the Institute’s Interventional Cardiology Sub-Division equipped with six x-ray labs for coronarography and spiral computer tomography, the resuscitation and observation division for the patients after coronarography and restoration of patency of the coronary arteries, the lecture room with back-up facilities and guest rooms and restaurant for guests and patients are located on the ground floor. The clinical and scientific laboratory, the tissue preservation and deep freezing laboratory with the bank of heart valves, ECG, Echo and Ergocardiometry laboratories, postoperative rehabilitation room, image documentation laboratory and a restaurant for the staff are located on the first floor. The cardiac surgery division with the capacity of 100 beds in on the second floor. Europe’s unique, fully equipped and monitored postoperative intensive care unit with the capacity of 50 beds and surgical and operative back-up facilities is located on the third floor. The fourth floor is occupied by super modern operating ward with six operating theaters furnished with the latest cardiac surgery apparatus as well as the monitors and video cameras to enable a live transmission of cardiac surgery in the lecture and seminar rooms and a satellite broadcast to other continents.
The surgeons spend more than half of their lives in operating rooms without any access to daily light. Therefore, the walls have been covered with panels lit by natural daylight with beautiful colorful photos made by the team during their scientific journeys all around the world. The rooms bear the names according to the photos: “By the Parrots,” “Palm,” “Highland,” “Inca,” “Waterfalls,” and “Oriental.” The patients are able to choose their “favorite” operating room.
The extracorporeal circulation laboratory, heart-lung machine storage place (parking maszyn sztucznych płuco-serc) is divided into the so-called dirty and sterile parts so that human life can at any time be saved using circulation support or full extracorporeal circulation. The fifth floor is occupied by engine rooms and air conditioning equipment, which pumps the sterile air into the operating rooms and divisions. Technical equipment, computerized central sterilization and social back-up facilities with a cloakroom for the staff are located on the entrance level. Each floor contains a large hall with furnished niches where the patients can see the visitors.
The new cardiac surgery department began its activities in January 1998. The patients were transferred from the old and small facility to five times bigger new department and the staff began to work in truly European conditions. However, the expectations have grown and today the facility is too small! One hundred times bigger area proved too small for the laboratory which initially was located in the old building’s corridor.
In 1998, the number of surgeries performed daily increased and hit 25 and one night saw as many as three heart transplantations. In 2000, 3000 surgeries, including 2480 operations under extracorporeal circulation, and 70 heart transplantations were performed. 15,000 coronarographies and restorations of patency of coronary arteries using angioplasties and stents were performed at the Interventional Cardiology Institute. Potentially, 3000 cardiac surgeries and 30,000 coronary angiographies and angioplasties and vascular procedures could be performed annually. Such needs have in fact arisen but unfortunately they are hampered by the financial incapacity of the National Health Fund. The Cardiac Surgery Department in Cracow has become the pride and distinctive feature of the city and the center for the transmission of progress from the West to the East. It trains the specialists from Eastern Europe and performs demonstrative cardiac surgeries during the scientific sessions held behind the Eastern border.
The old building of the cardiac surgery department has undergone a radical modernization and emerged as a modern facility with one extra floor. The admission room No. 2 for the patients of the Department of Interventional Cardiology, two cathlabs to perform coronaroraphy, patient observation room and the operating room where pacemakers are implanted are located on the ground floor. On the first floor, there is the vascular surgery division and echocardiography laboratory. The second floor comprises the division for the patients before and after heart transplantation. The fourth floor is occupied by two super modern, air-conditioned operating rooms for transplantation purposes. Next to it, there is the intensive care unit for the patients after heart as well as heart and lung transplantations with the capacity of 15 beds.
In the upgraded old and new facility, the Cardiovascular Surgery and Transplantology Department of the Jagiellonian University Collegium Medicum at John Paul II Hospital enjoys optimum conditions of treatment and scientific development, now under supervision of Prof. Jerzy S. Sadowski, who took the chair after me in 2001 (Figs 40 and 41).
 |
| Fig. 40. “The exchange of generations” at the Dept. of Cardiac Vascular Surgery and Transplantology in 2001. At this celebration Prof. Antoni J. Dziatkowiak passes to his pupil successor, Prof. Jerzy Sadowski, his surgical post and symbolic “Golden Scalpel” and transient “Golden Needle-Holder” he got from Prof. Jan Moll when he was leaving ŁódĽ in 1979. |
 |
Fig. 41. Prof. Jerzy S. Sadowski, head of the Dept. of Cardiovascular Surgery and Transplantology and vice-director of Institute of Cardiology, Collegium Medicum, Jagiellonian University since 2001. |
At the ceremony of the Inauguration of Academic Year 2000/2001 I had been decorated with “Grand Cross” of the Order of Poland’s Restitution (Fig. 42).
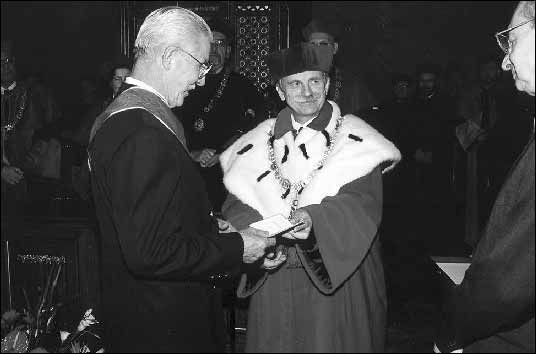 |
| Fig. 42. At the inauguration ceremony of the academic year 2000/2001; Prof. Franciszek Ziejka - His Magnificence Rector of the Jagiellonian University, and Mr Zdrada, the Minister of Education decorate Prof. Antoni J. Dziatkowiak with the highest Polish State Award “Grand Cross” of the Order of Poland`s Restitution. |
During the two International Cardiac Surgery Congresses organized in 1986 (Fig. 43) and 2000 in Cracow (Fig. 44) by the cardiac surgery department of Cracow, the participants and the board of the Association of Polish Surgeons (the thoracic and cardiac angiosurgery was a section of the abovementioned Association) were convinced about a high level of the Polish cardiac surgery, its scientific and staff potential, its maturity and its readiness to make independent decisions. I included the motion to establish the independent association of cardiac surgeons in the agenda of the general assembly of the Chest, Cardiac and Vascular Surgery Section. With great respect to the achievements of the Association of Polish Surgeons over the past one hundred years and the experience of 29 subsequent symposia and congresses of the Chest, Cardiac and Vascular Surgery Section, the cardiac and thoracic surgeons became convinced they could become separated from the structures of the Association of Polish Surgeons. The Polish Association of Cardiac and Thoracic Surgeons was established at the next 29th congress of the Section held in 2002 in Szczecin. It issues its own quarterly entitled Polish Cardiac and Thoracic Surgery. The Polish Association of Vascular Surgery was separated a year earlier.
 |
| Fig. 43. Dr Hans Borst of Hannnover - an invited speaker at the 21st Int. Congress of Thoracic and Cardiovascular Surgery in Cracow 1986. |
 |
| Fig. 44. The outstanding cardiac surgeon of Beograd, Prof. Michailo Vucinic with his wife Lucija at 28-th Int Cardio-Thoracic Congress in Cracow 2000. |
The Club of Polish Cardiac Surgeons comprising the heads of the country’s departments and cardiac surgery divisions was established in 1983, during the martial law, at the initiative of Marian ¦liwiński. It is the informal, unregistered and voluntary association of the founding cardiac surgeons and one can get invited upon the recommendation of the Club’s member. The admission procedure is preceded by the announcement made by an invitor and a member is admitted by the majority of votes cast in a secret ballot. As the Club has not been registered, it cannot be dissolved by the state authorities. The Club’s activity is based on the old and respectable tradition of the Polish academic surgery, reliability, truthfulness, friendship and the observance of rules governing the conduct for the benefit of a patient, development of cardiac surgery and cardiac surgeons. The Club maintains the reports and carries out an annual thorough analysis of achievements of the Polish cardiac surgery to be used by the authorities and the European Commission, organizes specialist trainings and provides the assistance related to the habilitation theses. Chaired by Marian ¦liwiński, the Club’s meetings have already been convened 55 times (Fig. 45). The positive role played by the Club consists, inter alia, in a group pressure exerted on state authorities to obtain funds to purchase the equipment and life saving drugs and agents. Today, it represents the environment in essential negotiations concerning the prophylaxis and treatment of cardiovascular system diseases and the distribution of funds to finance the abovementioned program. After 22 years of the Club’s activity, it can be said it has made a remarkable contribution to the development of the Polish cardiac surgery, which is best manifested by the following achievements recorded over the past 20 years: from 1800 to 30,000 cardiac surgeries a year, over 1000 heart transplantations, increase in the number of specialists and assistant professors and change in the physicians’ attitude – do not wait until cardiac infarction develops or expands and promptly, during the so-called golden hour, restore the patency of the occluding coronary artery or perform coronary artery bypass grafting! Do not waste time for complex diagnostics of acute dissection of the ascending aorta, promptly place the patient on the operating table and, following the administration of an anesthetic, perform transesophageal echocardiography, which confirms the suspected ailment in 99%. In 1980, the average rate of death during the surgeries under extracorporeal circulation stood at 25%, in 2000 at 5% and today at 3%.
 |
| Fig. 45. The Club of Polish Cardiac Surgeons – the meeting in Mr±gowo in 2000. From the left: Janusz Zasłonka (ŁódĽ), Bohdan Szelagowicz (Poznań), Marian Sliwiński (Warsaw) (the President), Antoni J. Dziatkowiak (Cracow), Irena Smólska (Warsaw), Seweryn Wiechowski (Szczecin), Wacław Sitkowski (Warsaw), Zygmund Sadowski (Warsaw), Tadeusz Bross (Wrocław). |
THE GOLDEN SCALPEL is the most prestigious award granted by the Club to its members who made a particular contribution to the Polish cardiac surgery. I also had the honor to obtain such a reward.
The Polish pioneering cardiac surgeons included the outstanding general surgeons who were also engaged in thoracic and cardiac surgery but formally did not complete any specialization in cardiac surgery because at that time such a specialization did not exist. Their apprentices (today, the assistant professors and professors) also did not have any specialization in cardiac surgery but they nonetheless performed heart surgeries and organized the second degree specialization exams in cardiac surgery for the surgeons. The problem related to the failure to regulate the provisions was solved in 1993 with the state exam taken by all heads of departments and divisions engaged in cardiac surgery. The struggle with the clerks to define cardiac surgery as the chief specialization took more than 10 years and was concluded with the entry in the list of chief specializations equal to surgery and thoracic surgery. Today, we have 180 specialists in cardiac surgery and 80 potential cardiac surgeons who have not yet completed their specialization. In the country with almost 40 million citizens the abovementioned number is obviously too small especially given the fact that many physicians, given their poor wages, leave Poland to work in the West.
As regards the abovementioned fields, Poland has caught up with the West over the past 15 years. Today we perform all diagnostic examinations and apply all therapeutic methods that are performed or applied in the world. We have been well provided, especially in Cracow, with modern equipment including the latest generation magnetic resonance for spiral computer tomography. Our weak side is the inability to entirely use our skills given the insufficient amounts provided by the Polish health care system, which, as we all know, is the function of economy. The expensive, highly specialized procedures including the cardiological invasive procedures and cardiac surgeries are financed by the National Health Fund. It transfers the restricted amounts to finance the contracts, which are too small to meet the growing demands of the society.
This is the question! We would love our wise society to take the health issues also in their hands and prevent the diseases, at least cardiovascular system diseases, through pro-ecological development and wide-range preventive measures undertaken already in childhood. I am afraid, however, that this will not happen in foreseeable future. People will continue eating too much food, smoking cigarettes, taking drugs and sitting glued to TV or computer screens so the toll taken by atherosclerosis will force the cardiac surgeons to continue their activities. Moreover, a growing number of certain injuries and traffic accidents will be dealt with by the cardiac surgeons. I am deeply convinced that John Paul II Hospital will eventually assume the name adequate to its function, namely John Paul II Center of Heart and Lung Disease in Cracow - a reference center of Eastern Europe.
- American College of Cardiology. A Visual History 1949-1999. Library of Congress, Cat. No. 98-74461
- Antoszewski Z, Sych M.:Pozaustrojowe kr±żenie krwi i pozapłucne oddychanie (Extracorporeal Circulation and Respiration) PZWL, Warsaw 1984.
- Backer Ch, Brock RC, Campbell M. Valvotomy for Mitral Stenosis. Brit Med J. 1950; 6:
- Barta K, Brajer H. 50 lat Miejskiego Szpitala Specjalistycznego im Dr Anki w Krakowie (50 Years of Dr Anka Municipal Specialist Hospital in Cracow), WAG, Cracow 1968.
- Bigelow WG, Callaghan JC, Hoops JA. General Hypothermia for Experimental Intracardiac Surgery. Ann Surg 1950; 132: 3.
- Blalock A. Cardiovascular Surgery Past and Present. J Thor Cardiovas Surg. 1966; 52: 2.
- Bodnar E, Yacoub M. Biologic Bioprosthetic Valves. Yorke Med Books 1986.
- Bogusz J, Rudowski W. Sylwetki chirurgów polskich (The Silhouettes of Polish Surgeons), Zakład Narodowy im. Ossolińskich. Wyd PAN 1982.
- Bosrt HG, Klinner W, Sennig A. Herz und herznahe Gefasse. Springer Verl Berlin Heidelberg New York 1978.
- Bross W, Koczorowski S. Chirurgia klatki piersiowej (Chest Surgery). PZWL, Warsaw 1957.
- Brzezinski T. Historia medycyny (The History of Medicine). PZWL, Warsaw 1988.
- Crafoord C, Norberg B, Senning A. Clinical Studies in Extracorporeal Circulation with Heart-Lung Machine. Acta Chir Scand 1957; 38: 3-4.
- Dziatkowiak AJ. Pamiętnik Sympozjum Kardiochirurgicznego, ŁódĽ 6-7 IX.1972. Jubileusz 60-lecia urodzin prof. dra hab. med. Jana Molla (Memoirs of Cardiosurgical Symposium in ŁódĽ, Sept. 6-7, IX,1972 to Celebrate Dr Jan Moll’s 60th Birthday). ŁódĽ 1973.
- Dziatkowiak A, Paluch K. Kardiologia i Kardiochirurgia w Krakowie. Fundacja COR AEGRUM . Po¶więcenie nowej klinki kardiochirurgii przez papieża Jana Pawła II (Cardiology and Cardiac Surgery in Cracow. COR AEGRUM Foundation. Consecration of the New Cardiac Surgery Department by John Paul II). Cracow 1997.
- Dziatkowiak A, Tracz W. 25 lat Instytutu Kardiologii Collegium Medicum Uniwersytetu Jagiellońskiego 1979-2004 (25 Years of the Institute of Cardiology of Collegium Medicum of Jagiellonian University 1979-2004).
- Ellis H. Famous Operations. Harval Publ Co. Media PA, 1984.
- Grochowski J. Profesorowie, docenci, doktorzy habilitowani oraz doktorzy honoris causa Akademii Medycznej im. Kopernika w Krakowie w latach 1970-1980. (Professors, Associate Professors and Honoris Causa Doctors of M. Copernicus Medical University of Cracow in 1970-1980) Cracow 1981.
- Kardiochirurgia i Torakochirurgia Polska (Polish Journal of Cardio- Thoracic Surgery) 2004; l: 1: 4. 2005; 2:1, 2, 3.
- 25-lecie Instytutu Kardiologii Collegium Medicum Uniwersytetu Jagiellońskiego w Krakowie (Polish Heart Journal. 25 Years of the Institute of Cardiology of Collegium Medicum of Jagiellonian University in Cracow). Kardiologia Polska 2004; 61: Suppl. 2
- Kirklin JW, Barrat-Boyes BG. Cardiac Surgery. Churchill Livingstone Inc. N.Y.,1986.
- Kto jest kim w polskiej medycynie (Who is Who in Polish Medicine) Interpress, Warsaw, 1987.
- Kuch J, ¦ródka A. Dzieje Kardiologii w Polsce (History of Cardiology in Poland), PWN, Warsaw 1994 and 2004.
- Kuss R, Bourget P. An Illustrated History of Organ Transplantation. SANDOZ Lab., France1992.
- Lefrak EA, Starr A. Cardiac Valve Prostheses. Appleton-Century-Crofts, N.Y. 1979.
- May AA, Neville WE. Committee Communication, Surgery for Coronary Heart Disease 1969-1971. Chest 1973; 63: 4.
- Meade RH. Some of Forgotten Men in the Field of Thoracic Surgery. J Thor Surg 1956; 32: 2.
- Meissner RK, Hasik MJ. Polski wkład w medycynę ¶wiatow± (Polish Contribution to the World Medicine. KAW, Poznań 1989.
- Melrose DG, Dreger B, Bentall H.H. et al.: Elective Cardiac Arrest. Lancet 1955; 2: 21.
- Moll J. Działalno¶ć naukowa i lekarska (Scientific and Medical Activity of Dr Jan Moll). Włocławskie Tow. Naukowe 1984.
- Noszczyk W. Zarys dziejów chirurgii polskiej (Outlined History of Polish Surgery). PWN, Warsaw 1989.
- Pettersson G. et al. In Honor of Inge Haugdahl Rygg, Copenhagen 1993.
- Pasowicz M. Krakowski Szpital Specjalistyczny im. Jana Pawła II, 1917 – 2005 (John Paul II Cracow Specialist Hospital, 1917 – 2005). Cracow 2005.
- Religa Z. Zarys kardiochirurgii (Outline of Cardiac Surgery). PZWL, Warsaw 1993.
- Rudowski W. Album Chirurgów Polskich (Album of Polish Surgeons). PAN, Ossolineum 1990.
- Rzepecki W, Langner J. Chirurgia układu oddechowego (Respiratory System Surgery), PZWL, Warsaw 1979.
- Sabiston DC, Spencer FC. Surgery of the Chest. W.B. Sauners Co.1990.
- Sitkowski W, Szaginski W. Chirurgia serca (Cardiac Surgery). Pol Przegl Chir 1989; 61: 9.
- Skulimowski M. Facultas Medica Cracoviensis. Akademia Medyczna Cracow 1981.
- Snellen HA. History of Cardiology. Donker Acad. Publ., Rotterdam 1984.
- ¦liwiński M, Goryszewski G. Kardiochirurgia 2004, Klub Kardiochirurgów Polskich (Report of the Club of Polish Cardiac Surgeons` on Cardiac Surgery in 2004). Instytut Kardiologii, Warsaw 2005.
- Temple R. The Genius of China. 3,000 Years of Science, Discovery and Invention. Multimedia Books Ltd 1991.
- Tochowicz L.Zarys historii Krakowskiej Szkoły Medycznej w 600-lecie Uniwersytetu Jagiellońskiego (Outlined History of Cracow Medical School on the 600th Anniversary of the Jagiellonian University). Cracow 1962.
- Unger F. Report of the Institute for Cardiac Survey. Academia Scientiarum et Atrium Europeae Salisburgi. 1992.