Endoscopic arresting of bleeding from the alimentary tract allowed to reduce mortality, shortened hospitalization time and diminished the costs of treatment. Operational endoscopy includes the following methods of treatment: injection endoscopy, thermal contact methods, e.g. electrocoagulation, thermal probe and non-contact methods, e.g. YAG laser, argon laser, argon plasma coagulation (APC), mechanical methods, e.g. clip method (Fig. 1) and "banding" and a combination of the methods, i.e. so called combined therapy (4-10).
 |
| Fig. 1. Active bleeding ulcer and ulcer with stigmata of recent bleeding. Injection method stops bleeding |
Injection method involves injecting the bleeding blood vessel with vasoconstricting substances such as adrenaline 1:10000, absolute ethanol, 3% NaCl, thrombin, 1% polydecanol or tissue sclerotizing glues (Fig. 2). Hemostasis is achieved in three stages: first the injected substance exerts pressure on the bleeding vessel, then chemical inflammatory response is brought about and finally reflex vasoconstriction of the vessel occurs (4, 5, 11-14). Contact methods involve great precision as accurate contact of the applicator with the bleeding site is required. Argon plasma coagulation (APC) deserves special attention. Safe coagulation is possible down to 3 mm, does not require contact between the application probe and the bleeding site. It allows to coagulate big, hard to reach areas using no-touch technique; besides it is easily performed and cheap. The method is commonly used. However one of its drawbacks is the risk of excessive dilation of the tract during gas application. It is used not only to stop bleeding but also to destroy vascular changes like angiodysplasia, sometimes it supplements endoscopic polypectomy or local treatment of neoplastic changes (15-19). Essential operative endoscopic procedures also include arresting bleeding from the varicose veins of the esophagus and stomach fundus. Here polydecanol or tissue sclerotizing glues are injected aside mechanical - banding methods that apply rubber tourniquets around the bleeding varicose vein (Fig. 3) (20-24).
 |
| Fig. 2. Treatment of bleeding ulcer with clip method using metal clip. |
 |
Fig. 3. Banding as a mechanical method applied to treatment of esophageal varices bleeding. |
Theraputic endoscopy is also used in the treatment of numerous pathological conditions of the biliary tract and pancreas, e.g. endoscopic sphincterotomy. Oddi's sphincter is incised to restore patency or to widen the orifice of the common bile duct. Sphincterotomy is recommended in case of cholecystolithiasis, especially after cholecystectomy and prior to elective cholecystectomy to avoid choledochotomy, acute biliary pancreatitis, acute obturative cholangitis, inoperative cancer of the Vater's papilla as a palliative management and in case of pancreatic fistulas (Fig. 4) (25, 26).
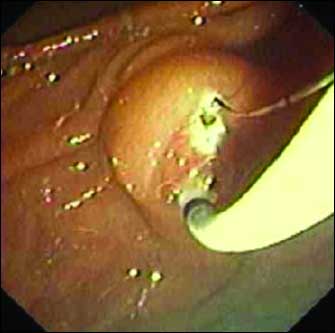 |
Fig. 4. Endoscopic sphincterotomy. The sphincterotome is inserted into common bile duct and cutting/coagulation setting is applied. Cut Vater's papilla is visible. |
Endoscopic sphincterotomy is a relatively safe procedure with 4 - 10% complications which include acute pancreatitis, acute cholangitis, bleeding and peripapillar perforation. Postoperative mortality does not exceed 1% cases. Contraindications to perform sphincterotomy are the same as to classic endoscopy of the upper regions of the alimentary tract. Additionally the method is contraindicated in case of impaired blood clotting and pancreatic cysts. Endoscopic sphincterotomy should not be undertaken if there is no possibility to perform direct drainage of the biliary tract or other therapeutic procedures required (27). Additionally Dormi's basket might turn useful after endoscopic sphincterotomy was performed in the patients with cholecystolithiasis when the concrements cannot be evacuated spontaneously from the common bile duct. Dormi's basket is used in case of single large-sized biliary calculi. Balloon occlusion method is used to remove numerous small-sized concrements from the common bile duct. Sometimes mechanical endoscopic lithotripsy, electrohydraulic or laser methods should precede Dormi's basket method (28, 29).
Modern operative endoscopy is also used in endoscopic prosthesis of the biliary and pancreatic tracts obstructed by unremovable biliary concrements, inoperative common bile duct stenosis of various origin, especially as palliative treatment of advanced stage cancers and for balloon dilatation of short common bile duct stenosis, both benign and malignant. Endoscopic prosthesis of the biliary tract is often undertaken in the patients with primary sclerosans cholangitis, especially when the patient waits for the liver transplant, in the patients with inoperative cancer of the Vater's papilla and in case of pancreatic fistulas. The procedure uses plastic prostheses of different length, diameter and shape (30).
Modern operative endoscopy is invaluable in the treatment of neoplastic changes, especially in the patients with advanced stage disease, when there is no chance for radical surgery. Here self-expanded metal prostheses are used to repair stenosis. They are particulary useful in case of esophageal cancer to ensure patency and to improve patient's comfort (30-34).
Polypectomy is a modern endoscopic procedure that can be applied to any part of the alimentary tract. It is considered to be a very important modality in operative endoscopy. It significantly decreases the development of neoplastic changes, especially those affecting the colon. It allows to resect the majority of stalked polyps, both single and multiple and large polyps by means of "bite" method (Fig. 5). Bleeding or perforation are possible side effects of the method. If the polyp stalk is very large or a big vessel is detected inside it, application of the clasp onto the polyp stalk might be useful in case of polypectomy to minimize the risk of bleeding (35-38).
 |
Fig. 5. Technique of endoscopic polypectomy. The polypectomy snare is looped around the stalk of the polyp. Next the snare is closed and polyp is removed by a blend of diatermic cutting and coagulation applied to the stalk. |
Mucosectomy is another endoscopic modality used to resect mucosa of the alimentary tract. It allows to remove large "sitting" changes, primarily benign though, sometimes early malignancies can be removed (Fig. 6). In Japan the method is commonly used to resect early neoplastic changes from the stomach and to treat of Barrett's esophagus (39-43).
 |
Fig. 6. Mucosectomy in the colon. The site after mucosa resection is visible |
Endoscopic dynamic phototherapy is based on fluorescein endoscopy. Photo sensitizer (generally 5-aminolevuinic acid) accumulates in the cancerous tissue; molecular oxygen and laser light trigger the release of free radicals and induce necrosis of the cancerous tissue. This method is indicated in case of inoperative cancer of the esophagus that obliterates its lumen completely and Barrett's esophagus. The method is tried in the treatment of colon and gallbladder cancers. Contraindications to endoscopic dynamic phototherapy include fistulas, tumors infiltrating blood vessels and porphyria.
Skin hypersensitivity is a considerable drawback that poses limitation to the method. Avoiding exposition to light is recommended for 4 - 6 weeks after the procedure. At present new agents are being searched that would not cause skin photo hypersensitivity or would shorten the photo hypersensitive effects to the minimum (44-50).
There has been enormous progress in operative endoscopy in the last years. It allowed among others internal drainage of the pancreatic pseudocysts by means of endosonography, the method that not long ago was considered only diagnostic.
- Konturek PC, Konturek SJ, Brzozowski T. Gastric cancer and Helicobacter pylori infection. J Physiol Pharmacol 2006; 57: 51-65.
- Konturek SJ, Konturek PC, Brzozowski T. Melatonin in gastroprotection against stress-induced acute gastric lesions and in healing of chronic gastric ulcer. J Physiol Pharmacol 2006; 57: 51-66.
- Brzozowski T, Konturek PC, Sliwowski Z et al. Interaction of nonsteroidal anti-inflammatory drugs (NSAID) with Helicobacter pylori in the stomach of humans and experimental animals. J Physiol Pharmacol 2006; 57: 67-79.
- Waterman M, Gralnek IM. Preventing complications of endoscopic hemostasis in acute upper gastrointestinal hemorrhage. Gastrointest Endosc Clin N Am 2007;17:157-167.
- Kovacs TO, Jensen DM. Endoscopic treatment of ulcer bleeding. Curr Treat Options Gastroenterol 2007; 10: 143-148.
- Lin HJ, Lo WC, Cheng YC, Perng CL. Endoscopic hemoclip versus triclip placement in patients with high-risk peptic ulcer bleeding. Am J Gastroenterol 2007;102:539-543.
- Kvan V, Norton ID. Endoscopic management of non-variceal upper gastrointestinal haemorrhage. ANZ J Surg 2007; 77: 222-230.
- Beejay U, Marcon NE. Endoscopic treatment of lower gastrointestinal bleeding. Curr Opin Gastroenterol 2002; 18: 87-93.
- Spinelli P, Calarco G, Manicini A, Ni XG. Operative colonoscopy in cancer patients. Minim Invasive Ther Allied Technol 2006; 15: 339-347.
- Konturek SJ, Konturek PC, Brzozowski T. Prostaglandins and ulcer healing. J Physiol Pharmacol 2005; 56(5) :5-31.
- Malara B. Josko J. Tyrpien M, Malara P, Steplewska K. Dynamics of changes in vascular endothelial growth factor (VEGF) expression and angiogenesis in stress-induced gastric ulceration in rats. J Physiol Pharmacol 2005; 56(2) :259-271.
- Konturek PC, Brzozowski T, Pajdo R et al. Ghrelin - a new gastroprotective factor in gastric mucosa. J Physiol Pharmacol 2004; 55(2) :325-336.
- Brzozowski T, Konturek PC, Konturek SJ, Brzozowska I, Pawlik T. Role of prostaglandins in gastroprotection and gastric adaptation. J Physiol Pharmacol 2005; 56(5): 33-55.
- Loster BW, Majewski JW, Czesnikiewicz-Guzik M, Bielański W., Pierzchalski P., Konturek SJ. The relationship between the presence of Helicobacter pylori in the oral cavity and gastric in the stomach. J Physiol Pharmacol 2006; 57(3): 91-100.
- Concha R, Amaro R, Barkin JS. Obscure gastrointestinal bleeding: diagnostic and therapeutic approach. J Clin Gastroenterol 2007; 41: 242-251.
- Sumiyama K, Kaise M, Kato M et al. New generation argon plasma coagulation in flexible endoskopy: ex vivo study and clinical experience. J Gastrointestinal Hepatol 2006; 21: 1122-1128.
- Goulet CJ, Disario JA, Emerson L, Hilden K, Holubkov R, Fang JE. In vivo evaluation of argon plasma coagulation in a porcine model. Gastrointest Endosc 2007; 65: 457-462.
- Meing A, Bajbouj M, Preeg M et al. Argon plasma ablation of gastric inlet patches in the cervical esophagus may alleviate globus sensation: a pilot trial. Endoscopy 2006;38:566-570.
- Manner H, May A, Faerber M, Rabenstein T, Ell C. Safety and efficacy of a new high power argon plasma coagulation system (hp-APC) in lesions of the upper gastrointestinal tract. Dig Liver Dis 2006;38:471-478.
- Habib A, Sanyal AJ. Acute variceal hemorrhage. Gastrointest Endosc Clin N Am 2007; 17: 223-252.
- Vitalis Z, Papp M, Tornai I, Altorjay I. Prevention and treatment of esophageal variceal bleeding. Orv Hetil 2006; 147: 2455-2463.
- Morales GF, Pereira Lima JC, Hornos AP et al. Octreotide for esophageal variceal bleeding treated with endoscopic sclerotherapy: a randomized, placebo-controlled trial. Hepatogastroenterology 2007; 54: 195-200.
- Mumtaz K, Majid S, Shah S et al. Prevalance of gastric varices and results of sclerotherapy with N-butyl 2 cyanoacrylate for controlling acute gastric variceal bleeding. World J Gastroenterol 2007; 13: 1247-1251.
- Singh H, Targownik LE, Ward G, Minuk GY, Bernstein CN. An assessment of endoscopic and concomitant management of acute variceal bleeding at e tertiary care centre. Can J Gastroenterol 2007; 21: 85-90.
- Costamagna G, Familiari P, Iacopini F, Shah S, Marchese M. State of the art in therapeutic biliary endoscopy. Rev Gastreoenterol Mex 2005; 70(suppl 1): 63-82.
- Guitron-Cantu A, Gutierrez-Bermudez JA. Therapeutic endoscopy in pancreas. Rev Gastroenterol Mex 2005; 70(suppl 1): 121-132.
- Rochester JS, Jaffe DL. Minimizing complications in endoscopic retrograde cholangiopancreatography and sphincterotomy. Gastrointest Endosc Clin N Am 2007; 17(1): 105-127.
- Papachristou GI, Baron TH, Gleeson F, Levy MJ, Topazian MD. Endoscopic retrograde cholangiopancreatography catheter and accessory exchange using a short hydrophilic guide wire: a prospective study. Endoscopy 2006; 38: 1133-1136.
- Mőssner J. Nutrition, probiotics, antioxidative therapy, endoscopy in chronic pancreatitis. Schweiz Rundsch Med Prax 2006; 95: 1627-1635.
- Farrell J, Carr-Locke D, Garrido T, Ruymann F, Shields S, Saltzman J. Endoscopic retrograde cholangiopancreatography after pancreaticoduodenectomy for benign and malignanat disease: indications and technical outcomes. Endoscopy 2006; 38: 1246-1249.
- Will U, Thieme A, Fueldner F, Gerlach R, Wanzar I, Meyer F. Treatment of biliary obstruction in selected patients by endoscopic ultrasonography (EUS)-guided transluminal biliary drainage. Endoscopy 2007; 39: 292-295.
- Ferrante M, Feliziani M, Imperatori A, Ferraris L, Bernasconi G. Endoscopic palliation of esophageal cancer. Rays 2006; 31: 3-7.
- Maerten P, El Wafa Abdou A, Kessler-Brondolo V, Doron M, Ortner MA. Contribution of endoscopy in palliative oncology (endoprotesis, photodynamic therapy, parenteral nutrition). Rev Med Suisse 2006; 2: 211-217.
- Konturek PC, Kania J, Burnat G, Hahn EG, Konturek SJ. Prostaglandins as mediators of cox-2 derived carcinogenesis in gastrointestinal tract. J Physiol Pharmacol 2005; 56(5): 57-73.
- Rubin PH, Waye JD. Colonoscopic polypectomy: a critical review of recent literature. Curr Gastroenterol Rep 2006; 8: 430-433.
- Frimberger E, von Deliuc S, Rösch T, Schmid RM. Colonoscopy and polypectomy with a side-viewing endoscope. Endoscopy 2007; 39: 462-465.
- Hernandez Guerrero A, Sorbino Cossio S. Therapeutic colonoscopy. Rev Gastroenterol Mex 2005; 70 (suppl 1): 149-157.
- Wei SC, Chang YT, Shieh MJ, Chang MC, Wang CY, Wong JM. The clinical and endoscopic characteristics, treatment and long-term prognosis of early colorectal in Taiwan. Dis Colon Rectum 2007; 50: 856-860.
- Deprez PH, Aouattah T, Piessevaux H. Endoscopic removal or ablation of esophageal and gastric superficial tumors. Acta Gastroenterol Belg 2006; 69: 304-311.
- Escourrou J. State of the art: endoscopic mucosal resection in Barrett. Rev Gastreoenterol Mex 2005; 70 (suppl 1): 25-34.
- Neuhaus H, Costamagna G, Deviere J et al. Endoscopic submucosal dissection (ESD) of early neoplastic gastric lesions using a new double-channel endoscope (the "R-scope). Endoscopy 2006; 38: 1016-1023.
- Annese V, Caletti G, Cipolletta L et al. Endoscopic treatment of gastroesophageal reflux disease. Endoscopy 2005; 37: 470-478.
- Picasso M, Blanchi S, Filiberti R, Di Muzio M, Conio M. Mucosectomy for high-grade dysplasia in Barrett's esophagus. Minim Invasive Ther Allied Technol 2006; 15: 325-330.
- Prasad GA, Wang KK, Buttar NS et al. Long-term survival following endoscopic and surgical treatment of high-grade dysplasia in Barrett's esophagus. Gastroenterology 2007; 132: 1226-1233.
- Mino-Kenudson M, Ban S, Ohana M et al. Buried dysplasia and early adenocarcinoma arising in Barrett esophagus after porfimer-photodynamic therapy. Am J Surg Pathol 2007; 31: 403-409.
- Shah AK, Wolfsen HC, Hemminger LL, Shah AA, DeVault KR. Changes in esophageal motility after porfimer sodium photodynamic therapy for Barrett's dysplasia and mucosal carcinoma. Dis Esophagus 2006; 19: 335-339.
- Ortner MA, Dorta G. Technology insight: Photodynamic therapy for cholangiocarcinoma. Nat Clin Pract Gastroenterol Hepatol 2006; 3: 459-467.
- Mordon S, Maunoury V. Using white light during photodynamic therapy: visualization only or treatment? Eur J Gastroenterol Hepatol 2006; 18: 765-771.
- Pech O, Gossner L, May A et al. Long-term results of photodynamic therapy with 5-aminolevuliniv acid for superficial Barrett's cancer and high-grade intraepithelial neoplasia. Gastrointest Endosc 2005; 62: 24-30.
- Maunoury V, Mordon S, Bulois P, Mirabel X, Hecquet B, Mariette C. Photodynamic therapy for early oesophageal cancer. Dig Liv Dis 2005; 37(7): 491-495.