The use of microvascular-anastomosed flaps
has become the gold standard for reconstruction of extended defects after tumour
ablation in head and neck area. Mainly applied flaps are the radial forearm
flap (rff), the lateral upper arm flap (luaf), the lateral thigh flap (ltf),
the latissimus dorsi flap (ldf) and the rectus abdominis flap (raf) (1- 4).
The advantage of the raf is that an extended tissue volume consisting of muscle,
subcutaneous fat and a variable big skin area with a reliable pedicle is available.
The skin area including the fat is nutrified
via separate perforator
vessels. These perforators are branches of the deep inferior epigastric artery
and vein. Therefore, the harvest of the deep inferior epigastric perforator
(DIEP) flap with extended skin-areas without sacrificing the
rectus abdominis
muscle is possible (5). High rates of successful reconstruction and little donor
site morbidity were pointed out in breast reconstruction with the DIEP (6, 7).
However there is very little experience with the DIEP in head and neck reconstruction
(8). We describe the technique of the DIEP for reconstruction of extensive voluminous
facial defects after ablative tumour surgery and its outcome in 10 cases.
PATIENTS AND METHODS
DIEP flap reconstruction for primary and secondary repair of large defects after
ablative tumour surgery was performed in 10 cases between 2001 and 2004 (follow
up between 12 and 47 month). The defect-locations, diagnoses of the tumours
and recipient vessels are specified in
Table 1 and
2. The resected
skin surface ranged between 40 and 180 cm
2. The
Ethic Committe of Dresden University approved this study and informed consent
was obtained from each patient.
| Table
1. |
 |
| Legend:
SCC - squamous cell carcinoma, NS - neurosarcoma, ChS - chondrosarcoma,
AcC - adenoidcystic carcinoma, FS - myxofibrosarcoma |
| Table
2. |
 |
Operation Technique
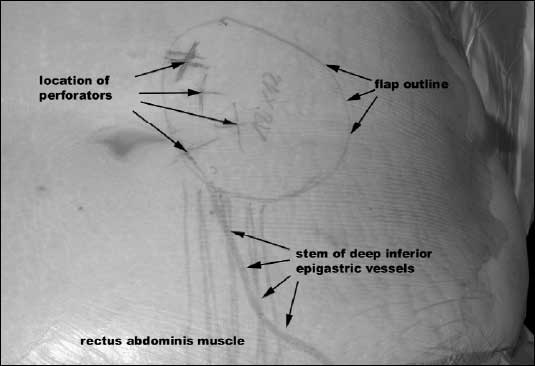
Preoperatively a Doppler flow imaging of the epigastric vessels was performed.
Hereby, the location and the calibre of the perforator vessels were assessed
and marked on the skin (
Fig. 1). Skin incision will then start at the
lateral part of the abdominal wall cutting through subcutaneous fat staying
on the fascia of the abdominal muscles. Without resecting any fascia the dissection
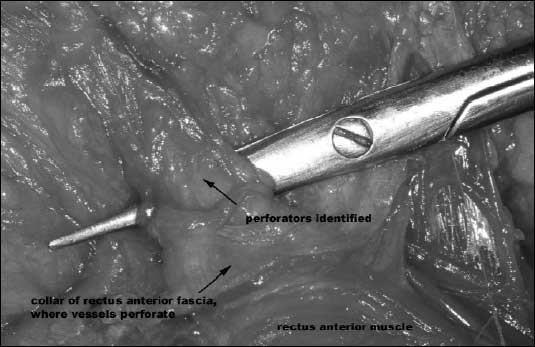
moves towards the midline. Once the selected periumbilical perforators are identified
(
Fig. 2), the
anterior rectus fascia is incised to form separate
collars around the tiny gaps to protect the perforating vessels. The incision
is then extended towards the groin to dissect the main stem of the inferior
epigastric vessels and to follow it to the level of the lateral border of the
rectus abdominis muscle. Then the branches leading from the inferior
epigastric stem to the perforator vessels are exposed by blunt dissection along
the muscle-fibres towards the tiny gaps in the fascia (
Fig. 3). Thereby
the motor-nerves are identified and because the pedicle is dissected deep to
motor nerves they can be mostly preserved. If this is not possible divided branches
are to suture. Thus, after completely developing the flap consisting of ligated
vessel pedicle, subcutaneous fat and skin, it is raised and transferred to the
recipient site. After the flap is sutured into the defect, the
A. and
V. epigastica inferior are connected to the recipient vessels by microsurgery.
Before wound closure at the donor-site the
rectus abdominis muscle and
the
anterior rectus sheath are inspected and potential surgical damages
to the structures is repaired by coaptation.
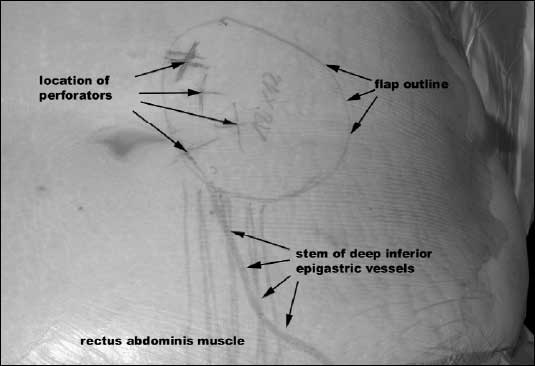 |
| Fig. 1.
Flap design and DIEP vessels outlined after Doppler-flow ultrasound investigation. |
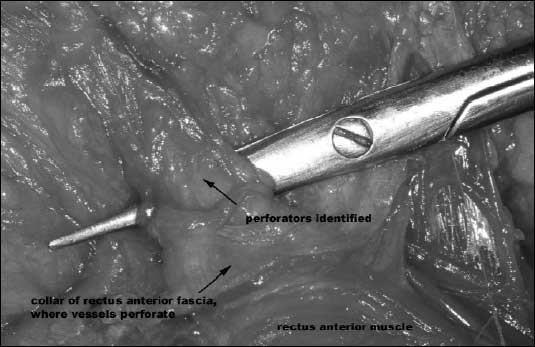 |
| Fig. 2.
Dissection of one large periumbilical perforator vessel embedded in a
collar of the anterior rectus fascia. |
 |
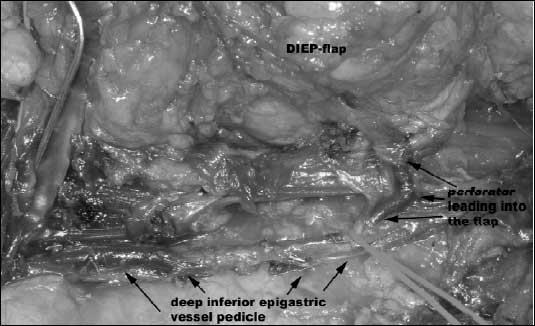
Fig. 3. Recipient sites of
DIEP-reconstruction (Patient 1 to 10). |
RESULTS
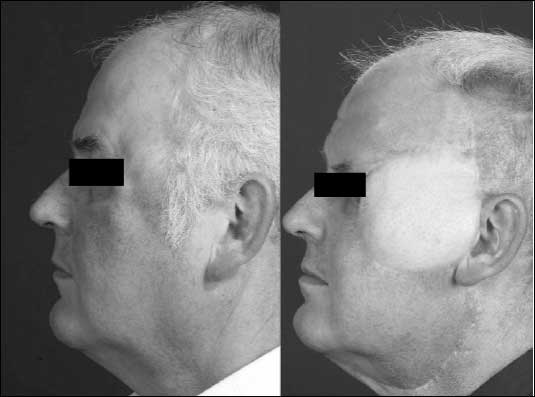
Nine of the 10 DIEP survived completely, 8 flaps healed uneventfully and without
any complication. A sufficient wound closure and aesthetically pleasing coverage
of the large facial defects could be achieved (
Fig. 4). A sufficient
healing also occurred in the 2 cases of secondary mandibular reconstruction.
Metal plates and free iliac bone grafts restored the continuities of the mandibles
and the DIEPs filled the extraoral soft tissue defects without complications
(
Fig. 5). In the patient who underwent a subtotal glossectomy a total
flap loss was encountered after thrombosis of the venous pedicle. It had occurred
after reintubation, necessitated by the threat of suffocation after pharyngeal
swelling. In one other patient primary skin closure of the tumour defect with
the flap could not be achieved due to bulky subcutaneous fatty tissue. The risk
to compress the vessel pedicle was avoided by temporarily covering a part of
the subcutaneous fatty tissue with Syspurderm
®
as artificial surface. After healing of the flap for 3 weeks, the adipose subcutaneous
tissue was reduced by liposuction and the defect area was closed completely.
Primary layered closure of the abdominal wall led in all cases to functional
and good aesthetic results of the donor sites. Abdominal wall complications
like bulking, herniation or functional deficits were not observed.
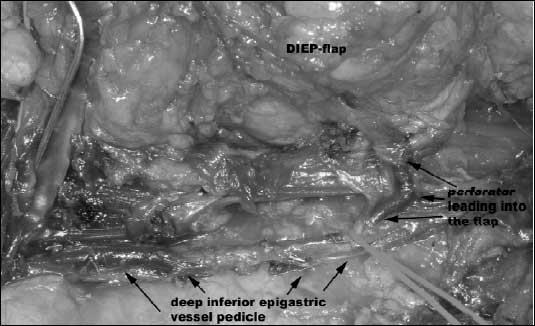 |
| Fig. 4.
Operation situs showing the vessel pedicle and a perforator leading into
the flap. |
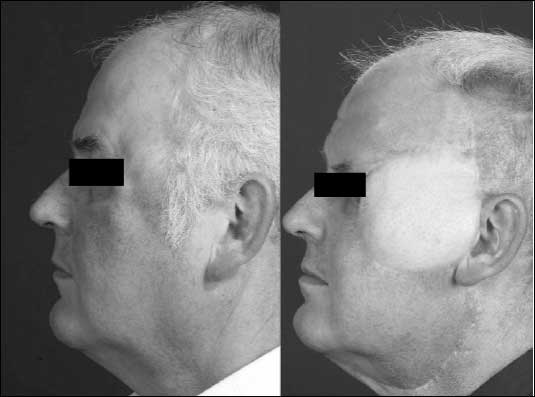 |
| Fig. 5.
Primary DIEP-flap reconstruction after resection of a myxofibrosarcoma
in the left temporal region |
 |
| Fig. 6.
DIEP-flap for soft tissue cover of free iliac bone graft in secondary reconstruction of the mandible after resection and radiation of a fibrosarcoma. |
DISCUSSION
Although the muscle-sparing DIEP-flap is widely used in breast reconstruction
surgery this report is one of the few of its application for large facial or
head and neck defect reconstruction (8-10). In general DIEP-flaps are very suitable
for the rehabilitation of large volume defects due to their pliable character
with a certain amount off subcutaneous tissue (9). The perforators provide a
good nutrition as a precondition for uneventful wound healing after successful
microvascular anastomosis at the recipient site. The importance of the perforators
blood supply is clearly demonstrated by the DIEP failure in this study, which
was encountered in the early postoperative interval. However, Moolenburgh
et
al. even described a DIEP failure 3 years after transplantation due to pedicle
diversion (11). In contrast to total flap loss Nahabedian
et al. reported
a rate of about 10% of fat necrosis related to breast reconstruction with DIEP-flaps
(12) and Kroll
et al. described a close relation between the size of
the perforators and fat necrosis (13). These facts relate to our experience
with the case of delayed primary defect closure after the liposuction. It suggests
that extensive subcutaneous fatty tissue due to adipositas should be encountered
as a risk factor for flap survival even when large perforators exist that guaranteed
well nutrified DIEP-flaps. All patients were satisfied with the aesthetic results
of the reconstruction and none of the patients showed functional disturbances
of the abdominal wall. The low donor site morbidity of the DIEP-flap except
the skin scar matches with the results of Blondeel
et al. who assessed
the function of the abdominal wall by clinical examinations, physical exercises
and a questionnaire after DIEP-and TRAM-flap elevation (14). However, the low
donor-site morbidity of the DIEP-flap is associated with a longer operation
time, due to the delicate dissection of the perforators to the stem of the deep
inferior epigastric vessels. This slight disadvantage is matched by the simultaneous
two-team approach for parallel flap harvesting and tumour-surgery as no patient
repositioning is required (15). Taken all this into account, we advocate the
DIEP as a reliable and save transplant for head and neck reconstruction.
The application of the DIEP-flap is in particular an alternative for primary and secondary reconstruction of large tumour associated defects in the head and neck area. Especially the pliability together with a certain volume, the long and reliable vascular pedicle and the texture of the flap make the DIEP suitable for the aesthetically challenging reconstruction of large facial defects after ablative tumour surgery. The preservation of the rectus abdominis muscle and the fascia guarantees a very little donor site morbidity. The simultaneous two-team approach for tumour surgery and flap harvesting makes the application of the DIEP very comfortable also for craniomaxillofacial or head and neck surgery.
Conflicts of interest statement: None declared.
REFERENCES
- Brown JS, Magennis P, Rogers SN, Cawood JI, Howell R, Vaughan ED. Trends in head and neck microvascular reconstructive surgery in Liverpool (1992-2001). Br J Oral Maxillofac Surg 2006; 44: 364-370.
- Lyons AJ. Perforator flaps in head and neck surgery. Int J Oral Maxillofac Surg 2006; 35: 199-207.
- Yokoo S, Komori T, Furudoi S et al. Indications for vascularized free rectus abdominis musculocutaneous flap in oromandibular region in terms of efficiency of anterior rectus sheath. Microsurgery 2003; 23: 96-102.
- Fanghanel J, Gedrange T, Proff P. The face-physiognomic expressiveness and human identity. Ann Anat 2006; 188: 261-266.
- Erni D, Harder YD. The dissection of the rectus abdominis myocutaneous flap with complete preservation of the anterior rectus sheath. Br J Plast Surg 2003; 56: 395-400.
- Gill PS, Hunt JP, Guerra AB et al. A 10 year retrospective review of 758 DIEP flaps for breast reconstruction. Plast Reconstr Surg 2004; 113: 1153-1160.
- Van Landuyt K, Blondeel P, Hamdi M, Tonnard P, Verpaele A, Monstrey S. The versatile DIEP flap: its use in lower extremity reconstruction. Br J Plast Surg 2005; 58: 2-13.
- Woodworth BA, Gillespie MB, Day T, Kline RM. Muscle-sparing abdominal free flaps in head and neck reconstruction. Head Neck 2006; 28: 802-7.
- Czesnikiewicz-Guzik M, Konturek SJ, Loster B, Wisniewska G, Majewski S. Melatonin and its role in oxidative stress related diseases of oral cavity. J Physiol Pharmacol 2007; 58: 5-19.
- Proff P, Weingärtner J, Fanghänel J, Gredes M, Mai R, Gedrange T. Regional changes in the masseter muscle of rats after reduction of blood supply. Ann Anat 2007; 189: 59-64.
- Moolenburgh SE, van Huizum MA, Hofer SO. DIEP-flap failure after pedicle division three years following transfer. Br J Plast Surg 2005; 58: 1000-1003.
- Nahabedian MY, Momen B, Galdino G, Manson PN. Reconstruction with the free TRAM or DIEP flap: patient selection, choice of flap, and outcome. Plast Reconstr Surg 2002; 110: 476-477.
- Kroll SS, Reece GP, Miller MJ et al. Comparison of cost for DIEP and free TRAM flap breast reconstructions. Plast Reconstr Surg 2001; 107: 1417-1418.
- Blondeel N, Vanderstraeten GG, Monstrey SJ et al. The donor site morbidity of free DIEP flaps and free TRAM flaps for breast reconstruction. Br J Plast Surg 1997; 50: 322-330.
- Trzcieniecka-Green A, Bargiel-Matusiewicz K, Borczyk J. Quality of life of patients after laryngectomy. J Physiol Pharmacol 2007; 58: 699-704.